When you find yourself asking, "is it ADHD or autism?", you're right at the heart of a very common and often confusing question. The key difference usually boils down to the why behind a specific behavior.
For instance, challenges seen in autism often come from a place of inherent differences in social understanding and a deep-seated need for routine. Similar struggles in ADHD, however, are typically fueled by issues with impulsivity and regulating attention.
Untangling ADHD and Autism: Answering the Core Question

Trying to figure out if certain behaviors point toward Attention-Deficit/Hyperactivity Disorder (ADHD) or Autism Spectrum Disorder (ASD) can feel like a tangled mess. So many of the traits look alike on the surface, which is exactly why self-diagnosis can be so tricky and why getting professional insight is non-negotiable.
The confusion is completely valid. Both are neurodevelopmental conditions, and it's even common for them to co-occur.
A good starting point for untangling them is to look at the primary motivation behind the actions. Think of it this way: two people show up late to a party. The person with ADHD might be late because they got completely sidetracked while getting ready and just lost track of time. In contrast, the autistic person might be late because the sheer anxiety of a new social situation made them delay leaving until they felt mentally prepared for it.
Key Behavioral Motivations
The reasons behind the behaviors offer the most valuable clues. While this is absolutely not a substitute for a professional diagnosis, understanding these different motivations can give you a much clearer framework.
- Executive Function Challenges: Both conditions can throw a wrench in executive functions like planning and organizing. In ADHD, this often looks like struggling to start a task or getting easily pulled off course. In autism, it might show up more as a difficulty with flexible thinking or smoothly transitioning from one activity to another.
- Social Interaction Differences: Someone with ADHD might interrupt others frequently, but it's driven by impulsivity—the thought just pops out. An autistic person, on the other hand, might struggle with the conversational back-and-forth because they process social cues and unspoken rules differently.
- Need for Routine: An autistic person often relies on predictability and routine to feel safe and grounded. A person with ADHD, however, may get bored with strict routines and actively crave novelty, even when they know a schedule would help.
A critical distinction often comes down to social motivation versus executive function. Autistic challenges are frequently rooted in a different way of processing social information, while ADHD challenges often arise from difficulties regulating focus, impulses, and energy.
To break it down even further, it can be helpful to see the core drivers side-by-side. While every individual is unique, this table offers a quick overview of the typical motivations behind common behaviors.
Quick Guide to Core Differences ADHD vs Autism
| Core Area | Primary Driver in ADHD | Primary Driver in Autism |
|---|---|---|
| Social Difficulties | Impulsivity, inattention, or emotional dysregulation may lead to interrupting or missing social cues. | Inherent differences in understanding and navigating social norms, communication styles, and nonverbal cues. |
| Focus | Difficulty sustaining attention on non-preferred tasks; easily distracted by external stimuli or internal thoughts (hyperfocus is also possible). | Intense, deep focus on specific special interests; difficulty shifting focus away from these interests or toward non-preferred tasks. |
| Routines | May struggle to maintain routines due to boredom or forgetfulness, often craving novelty and stimulation. | A strong need for predictability and routine to reduce anxiety and sensory overload; change can be distressing. |
Looking at the "why" behind an action provides a much more nuanced picture than just observing the behavior itself. It’s this deeper level of understanding that helps clinicians differentiate between the two conditions and provide the right kind of support.
Defining ADHD Beyond Distraction and Fidgeting
When most people think of ADHD, they imagine a kid bouncing off the walls or a colleague who just can't seem to focus. While those images aren't entirely wrong, they're a tiny, oversimplified piece of a much larger puzzle.
At its heart, ADHD is a neurodevelopmental condition that stems from challenges with executive functions—think of these as the brain's air traffic control system. These functions manage everything from organization and emotional regulation to time management and impulse control. When they aren't working smoothly, it creates persistent, often frustrating, challenges in daily life. Getting a handle on these deeper aspects is key to figuring out if you're looking at ADHD or autism.
The Three Presentations of ADHD
ADHD isn't a single, uniform experience. Clinicians have identified three distinct ways it shows up, each with its own set of very real-world struggles.
-
Predominantly Inattentive Presentation: This is what many people used to call ADD. It’s less about visible hyperactivity and much more about an internal storm of distraction and a struggle to keep focus. Someone with this presentation might consistently miss key details on a work project—not from a lack of caring, but because their brain has trouble tuning out irrelevant thoughts and stimuli.
-
Predominantly Hyperactive-Impulsive Presentation: This is closer to the classic stereotype, but it's still widely misunderstood, especially in adults. Adult hyperactivity might not be running around a room. It often feels like an intense internal restlessness, a mind that never quiets down, or a constant urge to be doing something. Impulsivity can show up as blurting things out in conversations, making snap decisions, or finding it nearly impossible to wait your turn.
-
Combined Presentation: This is the most common type. An individual with a combined presentation deals with a mix of both inattentive and hyperactive-impulsive symptoms. They might struggle to organize a simple to-do list while also feeling like they're being driven by a motor, both physically and mentally.
The most important thing to understand is that ADHD is not a character flaw or a failure of willpower. It's a persistent pattern of inattention and/or hyperactivity-impulsivity that gets in the way of functioning and development, rooted in the brain's unique structure and chemistry.
For instance, someone with inattentive ADHD might be called "lazy" for not finishing a report, when in reality, they've spent hours staring at the screen, completely overwhelmed and unable to organize their thoughts to begin. At the same time, a person with hyperactive-impulsive ADHD might struggle in relationships because they interrupt constantly, speaking without a filter. Recognizing these nuanced situations is the first real step toward an accurate understanding.
Defining Autism Beyond Social Awkwardness
While ADHD is often defined by its impact on executive functions, Autism Spectrum Disorder (ASD) is fundamentally about experiencing and processing the world in a completely different way. If you're asking, "is it ADHD or autism?", you have to look past the common stereotype of social awkwardness to find the real answer.
Autism is identified by a specific combination of traits that fall into two main categories. The first involves persistent differences in social communication and interaction. This isn't about being shy or intentionally rude; it’s about having different neurobiological wiring for how you engage with others.
For instance, an autistic person might communicate in a very direct, literal way and find it difficult to pick up on sarcasm or unwritten social rules. Others can easily misinterpret this, but it comes from a brain that processes information more concretely, not from a lack of care or empathy.
The Importance of Routine and Special Interests
The second key area involves restricted or repetitive patterns of behavior, interests, or activities. This is another widely misunderstood part of autism that is actually crucial for creating a sense of safety and structure.
These behaviors often include:
- A profound need for routine: Predictable schedules and familiar environments help reduce anxiety and the mental effort needed to navigate the day. An unexpected change isn't just an inconvenience—it can be deeply distressing.
- Deep, passionate special interests: These are much more than simple hobbies. A special interest is an intense focus on a particular topic that brings immense joy, a sense of order, and deep expertise.
- Repetitive movements (stimming): Actions like hand-flapping, rocking, or fidgeting are often self-soothing behaviors. They're a practical way to help regulate an overstimulated nervous system.
The core of the autistic experience is not a deficit but a different way of being. Social communication differences, sensory sensitivities, and a need for routine are adaptations to a world that often feels overwhelming and unpredictable.
Sensory Processing Differences
A critical, and often defining, component of autism is sensory sensitivity. An autistic individual may have senses that are either heightened or dulled compared to a neurotypical person. Bright fluorescent lights might feel physically painful, the constant hum of a refrigerator can be impossible to tune out, or the texture of a certain fabric can be completely unbearable.
This sensory reality shapes every aspect of an autistic person's life, determining which environments feel safe and which trigger immediate overload and distress. Understanding this is key to telling autism apart from ADHD. While sensory issues can exist with ADHD, they are not a core diagnostic criterion like they are for autism.
If these traits feel familiar, exploring how to get tested for autism can be an essential step toward getting clarity and the right kind of support.
A Side-by-Side Comparison of Overlapping Traits
When you’re trying to figure out if it’s ADHD or autism, the most confusing part is how many of the outward behaviors look almost identical. Both conditions can impact social skills, focus, and routines, but the internal reasons for these actions are worlds apart. Getting to the heart of this ‘why’ is the key to seeing the distinction.
For instance, both an autistic person and someone with ADHD might have a hard time in a group conversation. The behavior—difficulty participating—is the same. The cause, however, is completely different. The person with ADHD might get sidetracked by something in the room or blurt out a thought because their impulsivity won’t let them wait. On the other hand, the autistic individual might be struggling to process rapid-fire social cues, follow unspoken turn-taking rules, or feel overwhelmed by the noise.
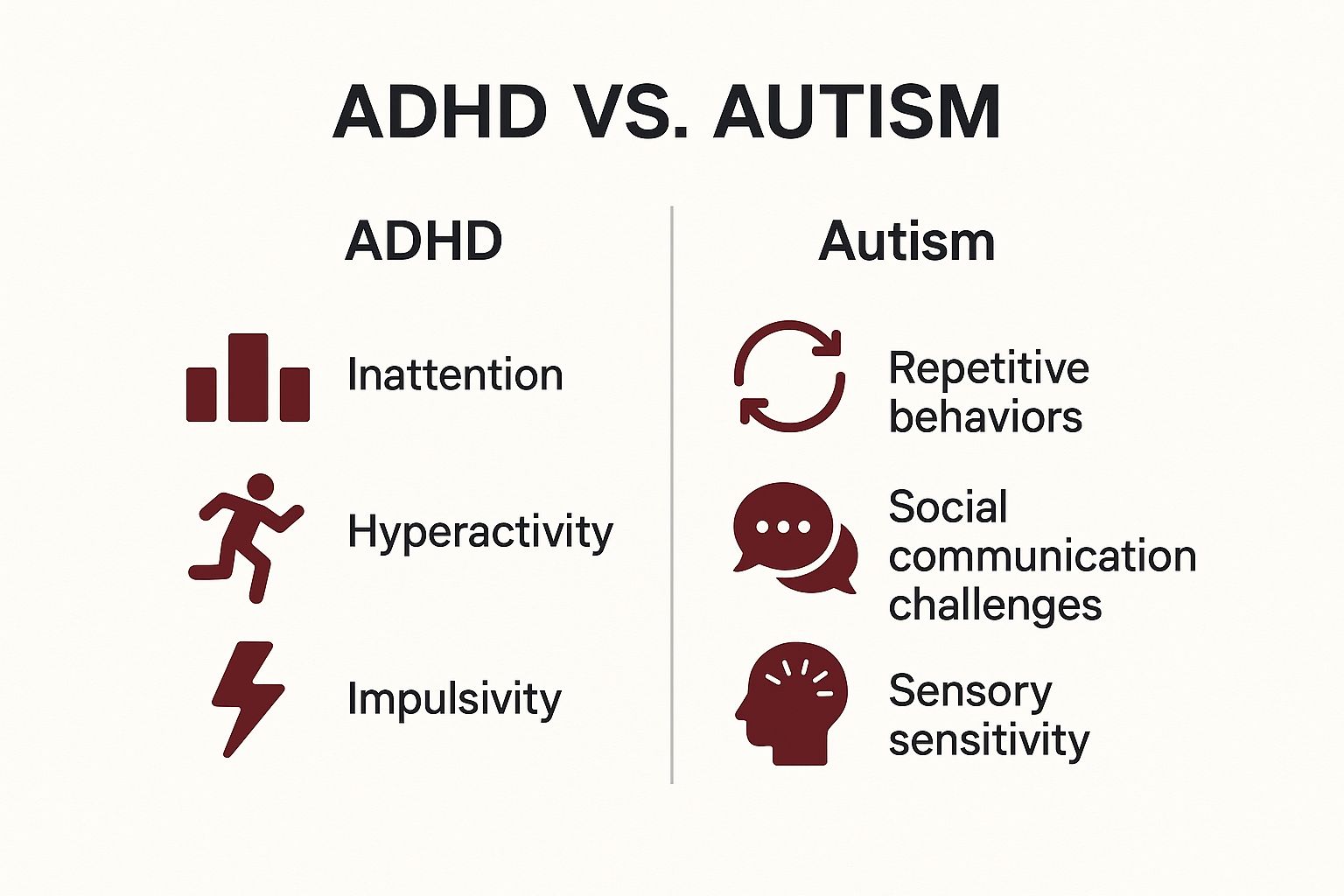
This infographic gives a great high-level view of the core diagnostic areas for each condition.
The image neatly separates the foundational traits of ADHD (inattention, hyperactivity, impulsivity) from those of autism (social challenges, repetitive behaviors, sensory sensitivity), which really helps clarify their distinct diagnostic cornerstones.
To dig deeper, this table breaks down how some of these similar-looking behaviors show up differently based on their underlying cause.
Side-by-Side Symptom Comparison ADHD vs Autism
| Behavioral Domain | Manifestation in ADHD | Manifestation in Autism |
|---|---|---|
| Social Interaction | Knows social rules but struggles to follow them due to impulsivity (interrupting) or inattention (drifting off). | May not intuitively grasp unwritten social rules or finds them illogical; prefers direct, literal communication and can miss subtle cues. |
| Attention & Focus | Experiences hyperfocus on novel, stimulating tasks. Attention can be hard to direct and is often pulled by external distractions. | Develops deep, long-term special interests. Focus is passionate and sustained, providing structure, joy, and expertise. |
| Routines & Sameness | Struggles to maintain routines due to a craving for novelty and dopamine. Can find repetitive tasks boring and draining. | Thrives on predictable routines for a sense of safety and to manage anxiety. Unexpected changes can be highly distressing. |
| Repetitive Movements | Fidgeting or restless movements (stimming) often serve to release excess energy or improve focus. | Repetitive movements (stimming) are typically used for self-regulation, expressing joy, or managing sensory input. |
Understanding these nuances is crucial because a diagnosis for either condition relies heavily on expert clinical observation—there’s no simple lab test to tell them apart.
Contrasting Social Interaction Styles
Social difficulties are a hallmark of both ADHD and autism, but they spring from entirely different sources. This is one of the most important distinctions to grasp.
- ADHD Social Challenges: These are often a direct result of executive function issues. Someone with ADHD might interrupt others, not because they’re rude, but because poor impulse control makes it feel impossible to hold a thought. They might seem checked out of a conversation because their attention has simply drifted elsewhere.
- Autism Social Differences: These come from a fundamentally different way of processing social information. An autistic person often prefers direct, literal communication and can miss the subtext in things like sarcasm or body language. Their challenges are rooted in navigating a neurotypical social world that runs on a completely different set of unwritten rules.
The key takeaway is this: An ADHDer often knows the social "rules" but struggles to follow them due to impulsivity or inattention. An autistic person may not intuitively grasp those same rules in the first place, or they may find them illogical and draining to follow.
The Nuances of Focus and Attention
Both ADHD and autism involve unique patterns of attention, though how that focus is directed and sustained is quite different. The term "hyperfocus" gets used for both, but it really describes two distinct experiences.
For someone with ADHD, hyperfocus is often an effortless, all-consuming state of concentration on something highly stimulating or new. It can be tough to control or direct, and it’s common to "snap out of it" and realize hours have flown by.
For an autistic person, this intense focus is better described as a special interest. This is a deep, passionate, and sustained fascination that brings joy, structure, and often, a high level of expertise. Unlike ADHD hyperfocus, which can be more random, a special interest is a core part of an autistic person's identity and a primary way they engage with the world.
Routines and Repetitive Behaviors
The approach to routines is another area where the underlying motivations couldn't be more different, offering a clear point of contrast.
- ADHD and Routines: Someone with ADHD might struggle to stick to a routine because they find it incredibly boring. Their brain is wired to seek novelty and dopamine, so repetitive tasks feel draining. It’s not uncommon for them to create elaborate routines, only to abandon them a week later.
- Autism and Routines: In contrast, an autistic person often thrives on routine and predictability. Routines create a sense of safety, reduce anxiety, and help manage an overwhelming sensory world. An unexpected change to a routine isn't just an annoyance—it can be extremely distressing and dysregulating.
This distinction is so important because, as mentioned, diagnoses rely on clinical observation. The significant symptom overlap can easily lead to misdiagnosis, an issue that's well-documented. According to the U.S. CDC, the diagnostic challenge is very real, and global inconsistencies in reporting underscore the need for specialized clinical expertise. You can learn more about the complexities of telling ADHD and autism apart from the CDC's latest research.
When It’s Both ADHD and Autism
For many people, the question isn't "is it ADHD or autism?" because the answer isn't a simple either/or. It’s not just possible to be both autistic and have ADHD—it’s actually quite common. Until 2013, the official clinical guidelines didn't even allow for a dual diagnosis, which forced people into a diagnostic box that never quite fit.
Now, we finally recognize this common co-occurrence, often called AuDHD. This term validates the experiences of countless individuals who see themselves reflected in both profiles but feel that neither one, on its own, tells the whole story. Understanding this overlap is absolutely crucial because it changes everything about diagnosis and support.
The Unique Experience of AuDHD
Living with AuDHD can feel like a constant internal tug-of-war. The autistic part of the brain often craves predictable routines and familiar, safe environments. At the very same time, the ADHD brain is chasing novelty and stimulation just to stay engaged and regulated.
This creates a deeply personal and often confusing internal conflict. For example, an AuDHD individual might impulsively book an exciting last-minute trip—satisfying that ADHD drive for novelty—only to feel completely overwhelmed by the disruption to their routine and the sensory chaos of travel, which triggers their autistic sensitivities.
The core challenge of AuDHD is managing two competing sets of needs. What soothes the autistic part of the brain can feel intensely boring to the ADHD part, and what stimulates the ADHD brain can be deeply dysregulating for the autistic side.
This internal push-and-pull can make daily life feel incredibly draining. You might find yourself creating new, elaborate routines that you absolutely love, only to abandon them a week later out of pure boredom. This cycle can exhaust your social battery, derail household chores, and lead straight to burnout. Getting a comprehensive evaluation is critical, as a professional can help untangle these competing traits. To learn more about how this works, you can explore what an ADHD and autism diagnosis actually entails.
The Importance of a Combined Diagnosis
The co-occurrence of ADHD and autism isn't just an anecdotal observation; it's backed by solid research. One large-scale U.S. study revealed that ADHD rates are roughly 10 times higher in autistic adults than in the general population. That same study noted that while ADHD symptoms can sometimes lessen with age, they often stay significantly elevated in autistic adults, contributing to more complex health challenges down the line. You can read more about the research on high co-occurrence rates on chop.edu.
Because having both conditions creates such a unique profile, a diagnosis that only flags one can lead to support that just doesn’t work. A support plan built only for autism might completely miss the executive function and impulsivity challenges of ADHD. On the flip side, a plan just for ADHD may fail to accommodate the critical sensory needs and social processing differences inherent to autism.
An accurate AuDHD diagnosis is the key to creating a support system that addresses the whole person. It allows for an integrated approach—one that respects the need for routine while finding healthy ways to bring in novelty. This helps individuals navigate their unique neurotype with greater understanding and, most importantly, self-compassion.
How to Pursue an Accurate Diagnosis
If you think you or a loved one might have ADHD, autism, or both, the most important step you can take is to seek a professional evaluation. Going down the rabbit hole of online information can be a good starting point, but it's no replacement for a formal assessment from an expert. The journey toward a real answer begins with finding the right professional.
The best-qualified experts to diagnose these conditions are typically clinical psychologists or psychiatrists. It's absolutely vital to find a provider with specific experience in differential diagnosis—the process of telling apart two or more conditions that have similar symptoms. This skill is non-negotiable, especially for adults, since the traits can look very different from how they do in childhood.
What a Comprehensive Evaluation Involves
A thorough diagnostic process is far more than a simple checklist. It's a deep dive into your life experiences, both past and present. To make sure you get a precise diagnosis, whether for ADHD or autism, the evaluation must be truly comprehensive.
A proper assessment usually includes:
- A Detailed Clinical Interview: This is where you'll discuss your current challenges, your developmental history going all the way back to childhood, and your family background.
- Behavioral Assessments: You'll likely fill out validated self-report questionnaires created to measure specific traits tied to ADHD and autism.
- Observational Data: The clinician will pay close attention to your communication style, behaviors, and thought processes during the evaluation itself.
An accurate diagnosis hinges on a skilled clinician piecing together the full picture of your life. There’s no simple blood test or brain scan; the diagnosis comes from interpreting behavioral patterns and personal history within a clinical context.
This reliance on observation and clinical interpretation helps explain why prevalence rates for conditions like autism can vary so much across the globe. A 2023 meta-analysis revealed that while the global prevalence of ASD is around 0.72%, it’s reported as high as 1.12% in the USA, which is likely due to greater awareness and more accessible diagnostic services. You can read the full research about these prevalence findings on PMC.
Ultimately, being your own advocate is key. Prepare for your appointment by writing down specific examples of your challenges. If you're particularly concerned about adult ADHD, learning what a dedicated ADHD assessment for adults involves can arm you with the right knowledge. This ensures you can give the clinician the detailed information they need to reach an accurate conclusion.
Common Questions About ADHD and Autism
When you're trying to figure out the differences between ADHD and autism, a lot of questions come up. It's a confusing landscape, and getting straight answers is the first step to clearing up some of the myths and finding the right path forward.
Can You Outgrow ADHD or Autism?
Simply put, no. Neither ADHD nor autism is something a person just "grows out of." Autism is a lifelong neurotype—it’s how the brain is wired. While autistic people learn incredibly effective ways to navigate the world and develop coping strategies over time, the fundamental wiring doesn’t change.
It's the same story with ADHD. While the way it shows up can shift as a person gets older—for instance, the classic hyperactivity might quiet down in adulthood—the core struggles with executive functions like staying organized, managing time, and regulating emotions tend to stick around.
Is Misdiagnosis Common Between the Two?
Yes, unfortunately, misdiagnosis happens more often than you'd think. It's also common for a co-occurring diagnosis to be missed entirely, especially if the clinician isn't a specialist in this area.
It's easy to see how wires get crossed. An autistic person’s deep, focused passion for a special interest could look a lot like ADHD hyperfocus. On the flip side, an ADHDer’s social difficulties, which often stem from inattention or impulsivity, might be mistaken for the social communication differences seen in autism.
A thorough, nuanced evaluation that looks at the “why” behind each behavior is essential. This is the only way to get an accurate diagnosis and make sure traits aren't being chalked up to the wrong cause.
How Do Support Strategies Differ?
Because these are two different neurotypes, the support that works best needs to be tailored to the individual.
- For ADHD, support often looks like a combination of medication and coaching. The goal is to build practical skills around executive functions—things like planning, organization, and emotional regulation.
- For autism, support frequently centers on changing the environment. This could mean accommodations for sensory sensitivities, finding alternative ways to communicate, or building predictable routines to reduce stress.
When someone has both conditions, which is quite common, the best approach is an integrated plan that addresses both sets of needs at once. This ensures that the strategies for managing ADHD don't clash with the support needed for autism, and vice versa.