When a clinician evaluates someone for ADHD, they aren't just running through a simple checklist. They're using a comprehensive framework to make an accurate diagnosis, guided by the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). These guidelines are designed to ensure that an ADHD diagnosis is consistent, thorough, and based on persistent patterns of behavior that truly get in the way of daily life.
What Are the ADHD Diagnostic Criteria?
Think of the official ADHD criteria less like a pop quiz and more like a detective's guide for piecing together evidence. A formal diagnosis is a lot more involved than just recognizing a few familiar traits. It takes a qualified professional to conduct a deep dive into an individual's history and current struggles.
The core idea is that these symptoms aren't just occasional or situational. To meet the criteria, they have to represent a consistent pattern that significantly interferes with—or reduces the quality of—social, school, or work life. A key piece of the puzzle is that these behaviors must show up in two or more settings, like at home and at school, or at home and at work.
The Foundation of Diagnosis
This multi-setting requirement is non-negotiable, and for good reason. It helps clinicians tell the difference between ADHD and other issues that might cause similar behaviors in just one environment. For example, a child might seem inattentive at school because of a specific learning disability, or an adult might be distracted at work due to extreme stress—neither of which is ADHD.
A diagnosis isn't just about whether symptoms are present. It's about their pervasiveness and impact. The criteria are designed to identify when these behaviors cross the line from being an occasional nuisance to a clinically significant impairment that needs real support.
Our goal here is to offer a clear, supportive starting point for anyone trying to understand these criteria, whether it’s for yourself, your child, or another loved one.
Core Components of an ADHD Diagnosis
To get the full picture, a clinician uses the DSM-5 criteria as their roadmap. This process is more than just observation; it involves gathering information from multiple sources to make sure the diagnosis is solid.
The table below breaks down the essential elements a clinician considers during an evaluation.
| Diagnostic Component | What It Means | Why It's Important |
|---|---|---|
| Symptom Threshold | Does the person show enough symptoms from the core categories of inattention and/or hyperactivity-impulsivity? | This ensures the pattern is significant and not just a few isolated traits. |
| Age of Onset | Were several of these symptoms present before the age of 12? | This establishes ADHD as a neurodevelopmental condition that starts in childhood, even if it's diagnosed later. |
| Cross-Setting Impairment | Are the symptoms causing real problems in at least two different areas of life (e.g., school, home, work, social settings)? | This confirms the symptoms are pervasive and not just a reaction to a specific situation. |
| Functional Impact | Is there clear evidence that the symptoms interfere with or reduce the quality of daily functioning? | This is the key difference between having some ADHD-like traits and having a clinical disorder that requires support. |
| Rule Out Other Causes | Have other potential causes for the symptoms (like anxiety, depression, or learning disorders) been considered and ruled out? | This prevents misdiagnosis and ensures the treatment plan targets the right condition. |
This structured approach helps ensure every diagnosis is made thoughtfully, ruling out other possibilities and setting the stage for effective, personalized support.
The Evolution of Diagnosing ADHD
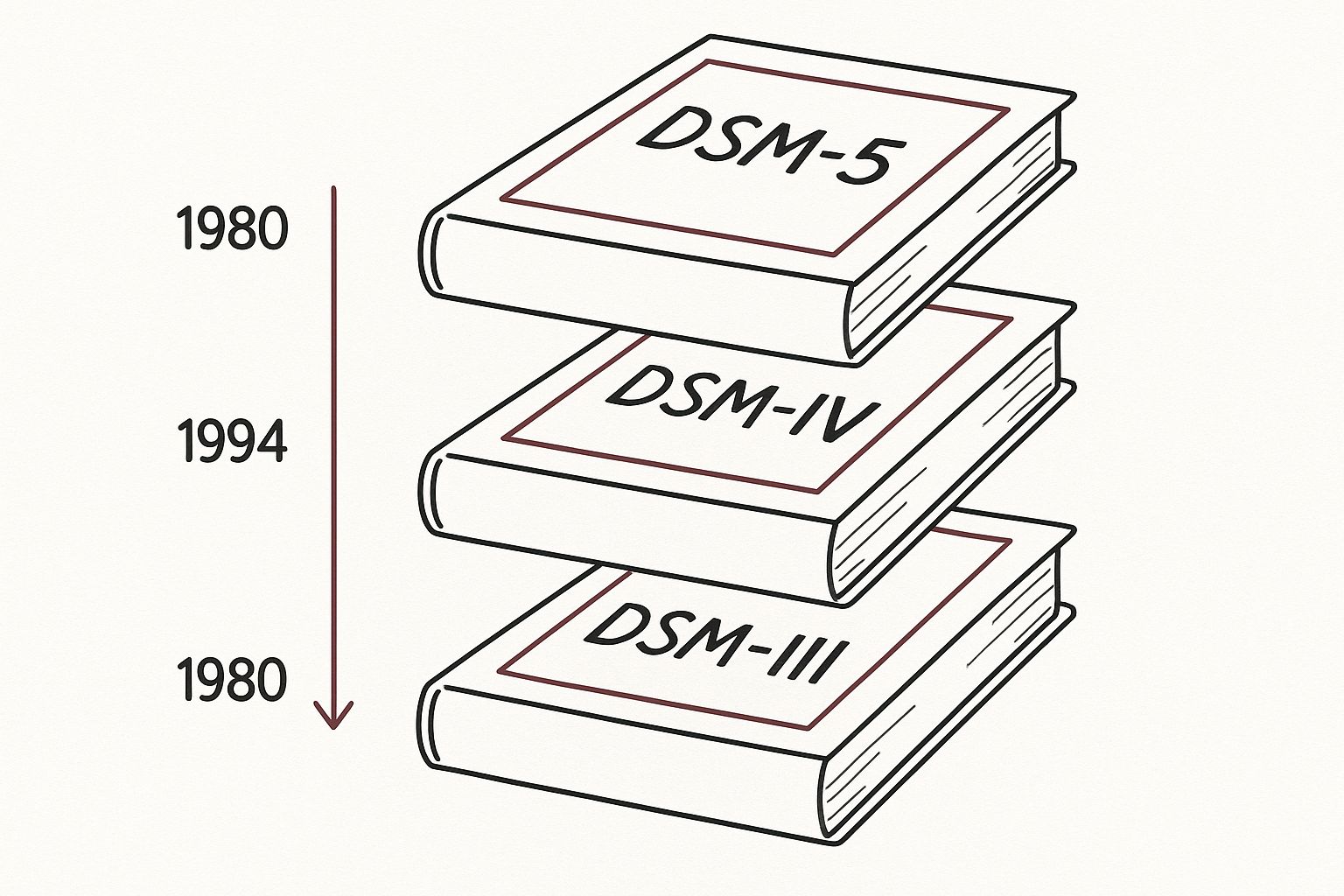
To really get a handle on today's ADHD diagnostic criteria, it helps to look back at how we've understood—and often misunderstood—the condition over time. The path from vague, early ideas to the specific, evidence-based guidelines we use now is a story of scientific progress and a much deeper appreciation for this complex neurodevelopmental disorder.
At first, the language was clunky and, frankly, a bit misleading. In the mid-20th century, behaviors we now link to ADHD were often chalked up to 'minimal brain damage' or 'minimal brain dysfunction.' These terms incorrectly suggested a physical brain injury. While this early thinking did start to frame these challenges as biological, the terminology wasn't clear enough for any kind of consistent diagnosis.
This infographic really captures the journey, showing how the diagnostic manuals have refined ADHD criteria over the decades.
You can see a clear shift from broad, sweeping categories to a much more nuanced view of ADHD's different flavors.
A Journey Through the DSM
The real game-changer was the Diagnostic and Statistical Manual of Mental Disorders (DSM). With each new edition, our understanding of ADHD sharpened, backed by a growing mountain of research. This evolution is key because it explains why today's criteria are structured the way they are.
The American Psychiatric Association's DSM gives us a clear timeline. Back in 1968, the DSM-II used the term 'Hyperkinetic Reaction of Childhood,' which focused almost entirely on hyperactive boys. This narrow lens meant countless people, especially those who were primarily inattentive, were completely missed.
The shift from focusing only on hyperactivity to recognizing inattention was a major breakthrough. It opened the door for diagnosing girls and adults who were previously overlooked because their symptoms didn't fit the classic "hyperactive boy" stereotype.
This wasn't the end of the story, of course. The diagnostic framework kept adapting as more evidence came in, leading to the more precise and inclusive criteria we have now.
From ADD to ADHD: The Three Presentations
In 1980, the DSM-III made a huge leap by introducing 'Attention-Deficit Disorder (ADD),' which could be diagnosed with or without hyperactivity. For the first time, inattention was officially on the map as a core component—a massive step forward. By 1987, the DSM-III-R revised the term again to 'Attention-Deficit Hyperactivity Disorder (ADHD),' cementing it as the primary name.
The modern framework we use today really took shape with the DSM-IV in 1994 and was carried into the current DSM-5. This model established the three distinct presentations of ADHD:
- Predominantly Inattentive Presentation: This is for individuals who mainly struggle with focus, organization, and finishing tasks.
- Predominantly Hyperactive-Impulsive Presentation: This is characterized by that classic restlessness, fidgeting, and acting before thinking.
- Combined Presentation: This is when a person meets the symptom criteria for both inattention and hyperactivity-impulsivity.
This history isn't just an academic footnote; it directly shapes how clinicians approach diagnosis today. Understanding this journey is vital for anyone seeking answers, and a professional evaluation is the best way to get them. To learn more about what a modern assessment involves, you might be interested in our guide on ADHD testing. This long progression ensures that a diagnosis today stands on decades of scientific refinement, giving you a solid foundation for getting the right support.
Decoding the Two Core Symptom Categories
When we talk about the ADHD diagnostic criteria, it's easy to get lost in checklists. To really get it, you have to understand the two pillars of the condition: Inattention and Hyperactivity-Impulsivity. These aren't just quirks or bad habits; they're the outward expression of a brain that's wired differently.
Let's start with inattention. It’s not about not caring. A great way to think about it is like trying to tune an old radio. You’re trying to lock onto a single station, but static and bits of every other channel are bleeding through all at once. The brain isn't choosing to ignore the important signal—it's just overwhelmed by all the other noise.
Then there's hyperactivity-impulsivity. This isn't a choice to be disruptive. Imagine you're behind the wheel of a sports car with a super-powerful engine, but the brakes are finicky and don't always engage when you press them. You want to slow down, but the car just doesn't respond in time. That's what it can feel like.
This section will unpack the specific DSM-5 symptoms for each of these categories, using real-world examples to show what they actually look like day-to-day.
The Inattentive Presentation
The inattentive side of ADHD is so much more than just daydreaming. It’s a chronic struggle with regulating focus and managing executive functions. For a formal diagnosis, a child needs to show at least six of these symptoms (or five for anyone 17 or older) for a minimum of six months.
What's tricky is that these symptoms can be subtle. They're easily overlooked, especially in quiet kids or high-functioning adults who have developed coping mechanisms.
- Makes careless mistakes or lacks attention to detail: This isn't just sloppiness. It's the student who totally gets the math concept but keeps making simple addition errors. It’s the professional who rereads an important email three times and still misses a glaring typo.
- Has trouble holding attention on tasks or activities: Think of the kid who dives into a Lego set with gusto, only to abandon it halfway through for something else. Or the adult who sits down to write a report and, ten minutes later, has 12 different browser tabs open on unrelated topics.
- Does not seem to listen when spoken to directly: Their mind is so full of that "radio static" that even when they’re looking right at you, the words don't always register. They aren't being rude; they genuinely didn't process it.
- Fails to finish schoolwork, chores, or duties in the workplace: This leads to a trail of half-done projects. The laundry gets washed but never folded, the work report is drafted but never finalized, and the dishwasher is loaded but never started.
- Has difficulty organizing tasks and activities: This is the messy backpack that seems to have a life of its own, the desk that’s buried under a mountain of papers, or the struggle to break a big project down into smaller, logical steps.
The core issue isn't a lack of desire to be focused or organized. It's a genuine executive function challenge that makes the act of planning, sequencing, and staying on task feel like climbing a mountain.
This constant mental effort is absolutely draining. Over time, it can take a real toll on a person's self-worth and ability to succeed at school or work.
The Hyperactive-Impulsive Presentation
This category is usually what people picture when they think of ADHD, but it's more complex than a kid who can't sit still. In adults, hyperactivity often turns inward, becoming a feeling of intense inner restlessness instead of constant motion. Just like with the inattentive criteria, a diagnosis requires at least six symptoms for kids (or five for those 17+) that have been present for at least six months.
Hyperactivity Symptoms:
- Fidgets with or taps hands or feet, or squirms in seat: In a child, it’s the non-stop wiggling. In an adult, it might be the foot that’s always bouncing under the conference table or the pen that’s constantly being clicked.
- Leaves seat in situations when remaining seated is expected: The child who can't stay at their desk grows into the adult who paces back and forth while on the phone or constantly finds reasons to get up from their desk at work.
- Is often "on the go," acting as if "driven by a motor": This is a profound, deep-seated feeling of needing to be in motion. For adults, this can look like overloading their schedule with projects or feeling deeply uncomfortable with any kind of downtime.
Impulsivity Symptoms:
- Blurts out an answer before a question has been completed: The brain is moving so fast that the answer pops out before the social brake has a chance to engage.
- Has trouble waiting their turn: This goes beyond simple impatience. It's a physical-feeling struggle against the powerful urge to act right now, whether that's in a conversation or waiting in line.
- Interrupts or intrudes on others: This comes from the same place. An idea or a thought feels so urgent that it completely bypasses the normal rhythm of a conversation.
Seeing these symptoms through the lens of everyday life helps shift the focus from a sterile checklist to a more compassionate understanding of the person behind the diagnosis.
Of course. Here is the rewritten section, crafted to sound like it was written by an experienced human expert.
How ADHD Symptoms Change Across a Lifespan
ADHD isn't a static condition that looks the same from one year to the next. It’s a neurodevelopmental disorder, which means it evolves and changes as a person grows. The way ADHD shows up in a seven-year-old can look completely different from how it presents in a thirty-seven-year-old. For this reason, the ADHD diagnostic criteria are flexible enough to account for how these core challenges manifest at different stages of life.
One of the foundational rules in the diagnostic manual is that several inattentive or hyperactive-impulsive symptoms must have been present before the age of 12. This isn't just an arbitrary cutoff. It’s a critical piece of evidence that helps a clinician see that the symptoms are part of a long-term developmental pattern, not something that cropped up in adulthood due to other issues like stress or anxiety.
Think of it like establishing a character's backstory in a film. A person's early experiences shape who they become later on. In the same way, identifying ADHD symptoms in childhood confirms the disorder's neurodevelopmental roots, even if a formal diagnosis doesn't happen until much later.
From External Hyperactivity to Internal Restlessness
The most dramatic shift in ADHD symptoms over time often involves hyperactivity. What is loud, obvious, and external in a child frequently becomes subtle, quiet, and internal in an adult. This is one of the main reasons so many adults with ADHD fly under the radar—their symptoms no longer match the classic stereotype of a kid who can't sit still.
For example, the overt hyperactivity of a child might look like:
- Constantly climbing on furniture or running through the house.
- Struggling to stay in their seat during class or at the dinner table.
- Acting as if they're "driven by a motor," with a relentless energy that wears out everyone around them.
As that child gets older, their brain develops more impulse control, but the underlying restlessness and need for stimulation don’t just vanish. Instead, they morph into more socially acceptable—and often invisible—forms of hyperactivity.
In an adult, that same hyperactive engine can manifest as:
- An intense, internal feeling of being unable to relax or "switch off" their brain.
- Constant fidgeting during meetings, like tapping a pen, shaking a foot, or picking at their nails.
- A tendency to be a "workaholic" or to always be on the go, feeling deeply uncomfortable with quiet downtime.
This internal restlessness is just as impairing as its external counterpart, but it's much harder for anyone on the outside to spot. It can lead to chronic stress, anxiety, and burnout as the adult constantly fights a feeling that their own mind and body are working against them.
The core challenge remains the same: a brain that's under-stimulated and is hunting for activity to compensate. The only thing that changes is how that need for stimulation is expressed as a person ages and learns to adapt to social norms.
Why the Symptom Threshold Is Lower for Adults
The diagnostic criteria also recognize these life-stage differences by adjusting the symptom threshold. For a child or adolescent to be diagnosed, they need to show six or more symptoms of either inattention or hyperactivity-impulsivity.
For anyone aged 17 and older, however, that threshold drops to five or more symptoms.
This isn't a random change; it’s based on solid clinical experience. By the time they reach adulthood, many people have developed sophisticated coping mechanisms to manage their most disruptive symptoms. They might have unintentionally gravitated toward careers that play to their strengths or built complex systems to make up for their weaknesses. These strategies can effectively mask some symptoms, making it seem like they have fewer than they did as a kid.
Lowering the symptom count to five acknowledges that the disorder is still present and causing real impairment, even if the adult has learned to camouflage some of its more obvious signs. This crucial tweak in the ADHD diagnostic criteria helps clinicians accurately identify adults who have struggled their whole lives without knowing why, finally opening the door for them to get the diagnosis and support they need.
The Real-World Impact of Evolving Criteria
Changes to the ADHD diagnostic criteria aren't just minor tweaks in a textbook; they have a real-world impact that changes lives. As the diagnostic manual has evolved alongside legal and social shifts, the way people are diagnosed, find support, and see themselves has been completely transformed. This has been a double-edged sword, bringing both incredible relief and sparking major public debate.
For many, this evolving understanding meant they finally got answers after years of struggling in silence. But on the flip side, it also fueled conversations about overdiagnosis, putting immense pressure on clinicians to apply the criteria with care and precision. Understanding this history is key to grasping what an ADHD diagnosis truly means today.
Increased Recognition and Access to Support
For decades, the common picture of ADHD was a hyperactive young boy. It was a narrow, limited view. That started to change as the diagnostic criteria broadened, especially with the DSM-III in 1980, to better capture inattention and how symptoms show up in adults.
This shift was supercharged by a major legal change in the U.S. In 1990, ADHD was included under the Americans with Disabilities Act, which provided crucial educational and legal protections. This created a much stronger incentive for diagnosis and treatment. As a result, between 1987 and 1996, the use of stimulant medication for children with ADHD jumped fourfold. You can find more details on these prevalence trends and their historical context in the full research paper.
This wasn't just about medication, though. It was about a massive leap in public awareness and clinical recognition. Suddenly, the diagnostic lens was wide enough to see the adults and adolescents who had been missed entirely.
The Debate Over Diagnosis Rates
Of course, the sharp rise in diagnoses sparked a debate that’s still going on. Many worried that the expanding criteria and growing awareness were leading to overdiagnosis—that kids were being medicated for behaviors that were just part of normal development. This concern really highlights how important it is for clinicians to conduct thorough, careful evaluations.
A proper diagnosis isn't a quick checklist. It involves ruling out other conditions, gathering a detailed personal history, and making sure the symptoms cause significant problems in more than one area of life. It’s a meticulous process designed to avoid mislabeling and get support to those who genuinely need it.
The tension between ensuring everyone who needs help gets it and preventing overdiagnosis is at the heart of modern ADHD care. This is exactly why sticking to the official ADHD diagnostic criteria is non-negotiable for clinicians and families.
This balancing act also shapes public perception. While more people getting diagnosed has been a lifeline for many, it has also fed skepticism and myths about the condition. If you're navigating a new diagnosis, it's so important to understand and overcome ADHD stigma, which often grows out of these public debates. The best defense we have against both under-recognition and overdiagnosis is the careful, professional application of the diagnostic criteria, ensuring every person's story is heard and understood correctly.
Navigating the Official Diagnostic Process
When you suspect you or a loved one might have ADHD, the path to getting clear answers can feel pretty overwhelming. The internet is flooded with quick online quizzes, but a real diagnosis is a much more thorough and structured process. Understanding what an official evaluation actually involves can take the mystery out of it and give you the confidence to seek out a high-quality assessment.
An official diagnosis based on the ADHD diagnostic criteria isn't a one-and-done event. Think of it more as a comprehensive investigation led by a qualified professional, like a psychologist or psychiatrist. They act like a detective, carefully gathering clues from different parts of your life to build a complete picture of who you are and what challenges you face.
The Clinical Interview and History
The first and most important step is a structured clinical interview. This is basically a detailed conversation where the clinician digs into your developmental, medical, and family history. They’ll ask about your experiences in childhood, your journey through school, your career path, and your social relationships. This deep dive is essential for establishing the long-term patterns of behavior that the diagnostic criteria require.
This focus on developmental history isn't new. Long before the current criteria were set, clinicians linked ADHD-like symptoms to subtle differences in motor skills and cognitive patterns. In fact, early research showed that specific motor examinations could reliably tell hyperactive children apart from their peers, which highlights how long we've known about ADHD's neurodevelopmental roots.
Using Standardized Rating Scales
Beyond the interview, clinicians use standardized, evidence-based rating scales. These aren't just simple questionnaires; they are scientifically validated tools created to measure the frequency and severity of ADHD symptoms.
Some common examples include:
- Conners Rating Scales: Often used for children and teens to get feedback from parents and teachers.
- Vanderbilt Assessment Scales: Another tool that gathers information from multiple people to assess symptoms and performance in different settings.
- Adult ADHD Self-Report Scale (ASRS): A screener and rating scale designed specifically for adults.
These tools provide objective data that helps the clinician see how your symptoms stack up against those of the general population. It adds a crucial layer of scientific rigor to the evaluation.
The Importance of Differential Diagnosis
One of the most critical parts of the whole process is what’s called a differential diagnosis. This is the clinical term for ruling out other conditions that can look a lot like ADHD. The truth is, many different issues can cause problems with focus, impulsivity, or restlessness.
A skilled clinician will carefully consider and rule out other possibilities, such as anxiety disorders, depression, learning disabilities, or even the effects of trauma. This step is essential to ensure you receive the right diagnosis and, consequently, the most effective treatment.
A proper evaluation is a collaborative and detailed process designed to give you clear, reliable answers. If you're thinking about taking this step, it helps to know what to expect from modern approaches. For a closer look at how this can be done conveniently from your own home, check out our guide on what a telehealth ADHD assessment involves.
Common Questions About an ADHD Diagnosis
Working your way toward a potential ADHD diagnosis can stir up a lot of questions. The sheer volume of information out there—some of it helpful, some of it not—can feel totally overwhelming. Let's clear up some of the confusion and tackle the most common questions people have about the ADHD diagnostic criteria and the evaluation itself.
Can I Have ADHD If I Did Well in School?
Yes, absolutely. It's a common misconception that ADHD and academic success can't coexist. Many people with ADHD, particularly those with the inattentive presentation or those who are intellectually gifted, become masters of compensation. They build incredibly effective coping strategies to get by.
You might have been that student who procrastinated until the eleventh hour but always managed to pull off a good grade through sheer force of will. While the outcome looks good on paper, it often comes at a huge personal cost. You may have had to work twice as hard or for much longer than your peers, leading to burnout and exhaustion. A proper diagnosis looks past the report card and considers the immense effort and impairment it took to get there.
Is an Online ADHD Test a Valid Diagnosis?
No. While those online quizzes and self-assessments can be a great starting point for recognizing your own symptoms, they can't give you an official diagnosis. Think of them like taking your own temperature—it gives you a data point, but it's not the same as a full medical work-up from a doctor.
A formal diagnosis must come from a qualified healthcare professional who conducts a comprehensive evaluation. This clinician will look at the whole picture: your symptoms, your life history, and, just as importantly, they'll rule out other conditions that can mimic ADHD.
Self-identification and finding community are incredibly powerful parts of the neurodivergent experience. However, a professional assessment is the only way to confirm a diagnosis and build a truly effective treatment plan that accounts for all the factors at play.
Why Do Symptoms Need to Be Present Before Age 12?
This is one of the most important criteria because ADHD is a neurodevelopmental disorder. That's just a way of saying its foundations are laid down in early brain development, and its effects are lifelong. By confirming that symptoms were present during this key developmental window, a clinician can more confidently distinguish ADHD from other issues that pop up in adulthood.
For instance, conditions like severe anxiety, depression, or the long-term effects of trauma can cause symptoms that look a lot like ADHD—think trouble concentrating or feeling restless. The "before age 12" rule helps ensure the challenges are part of a lifelong, developmental pattern, not a condition that emerged later.
Do I Need a Brain Scan for an ADHD Diagnosis?
A brain scan like an MRI or CT scan is not part of the standard ADHD diagnostic criteria. It's a common question, but the answer is a clear no for diagnostic purposes.
While advanced research imaging does show differences in brain structure and function between groups of people with and without ADHD, these findings aren't reliable enough to diagnose a single individual. The technology just isn't there yet. The diagnosis is made through a deep dive into your behavior, personal history, and how your symptoms impact different areas of your life, all guided by well-established clinical science.
At the Sachs Center, our expert psychologists provide comprehensive, telehealth-based evaluations for ADHD and Autism. We go beyond a simple checklist to give you the clarity you deserve. Learn more about our virtual diagnostic assessments and book your evaluation today.