Cognitive Behavioral Therapy, often called CBT, is a down-to-earth, goal-focused type of therapy. It zeroes in on the powerful link between what you think, how you feel, and what you do. The core idea is simple: by shifting unhelpful or negative thought patterns, you can change your feelings and actions for the better, leading to real improvements in your well-being.
Building a New Path for Your Mind
Think of your mind as having a well-worn trail that automatically leads to worry or sadness. When something stressful happens, your thoughts just naturally go down this familiar route, kicking off anxiety and making you want to avoid whatever is causing the stress. Cognitive Behavioral Therapy doesn't just point out that path; it hands you the tools to build a new, more constructive one.
CBT is less about deep dives into your distant past and more about tackling the challenges you're facing right now. It's a team effort between you and your therapist, where you work together to build a personalized "mental toolkit." This kit is filled with practical skills designed to help you spot, question, and reframe the automatic negative thoughts that often run on autopilot, just beneath your awareness.
A Practical and Evidence-Based Approach
Now, CBT isn't about slapping a layer of "positive thinking" on top of real problems or pretending they don't exist. It's more like becoming a detective of your own mind. You learn to examine the evidence behind your beliefs, questioning whether they're truly accurate.
A key insight you’ll gain is that it’s not the situation itself that causes distress, but your interpretation of that situation. By learning to see things from a more balanced and realistic viewpoint, you can dial down the emotional intensity and start making more deliberate choices.
This structured, skills-based method is one of the most thoroughly researched therapies out there. First developed back in the 1960s and 1970s, CBT is now a go-to treatment recommended in global health guidelines for conditions like anxiety and depression. Its success is backed by countless large-scale studies showing it helps a huge range of people, including many of the over 301 million people worldwide dealing with anxiety disorders. For a deeper dive, you can explore the latest trends in CBT research to see its impact.
The core idea of CBT is simple yet profound: You can gain control over your emotional well-being by learning to manage your thoughts and actions. It empowers you with the understanding that while you can't always control what happens to you, you can control how you respond.
This focus on actionable strategies makes CBT an incredibly effective way to create meaningful, lasting change and build up your resilience for whatever challenges come next.
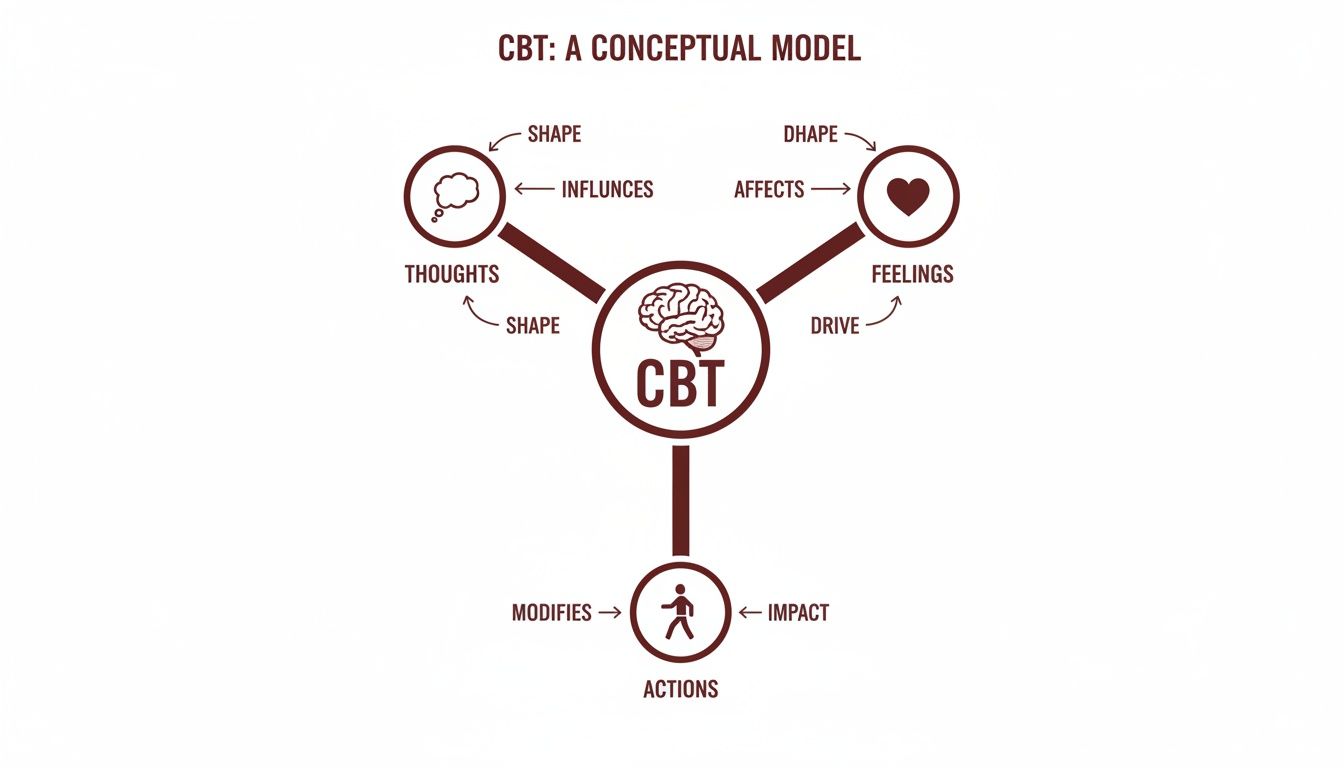
Understanding the Thought-Feeling-Behavior Triangle
At the very heart of CBT lies a simple but powerful idea: the cognitive triangle. This framework shows the direct, interconnected relationship between your thoughts, your feelings (emotions), and your behaviors (actions).
Think of it as a loop where each point influences the others. A situation itself is neutral—it's just a set of facts. What gives it meaning is the thought you have about it. That thought triggers a corresponding feeling, which in turn drives you to act in a certain way. This action often reinforces the original thought, locking you into a cycle that can be tough to break on your own.
The good news? An intervention at any point—whether changing a thought, managing a feeling, or altering a behavior—can disrupt the entire cycle.
Tracing the Cycle in Action
Let’s walk through a real-world example to see how this works. Imagine you have an important presentation coming up. The event itself is the neutral situation.
-
The Unhelpful Thought: An automatic thought pops into your head: "I am going to mess this up and sound stupid." This is a prediction, not a fact, but it feels incredibly real in the moment.
-
The Resulting Feeling: This thought immediately triggers feelings of intense anxiety and dread. Your heart might start racing, and you feel a knot in your stomach.
-
The Driven Behavior: Fueled by this anxiety, you might start procrastinating on your slides, over-preparing to the point of exhaustion, or deciding to stay silent during the Q&A to avoid saying the "wrong thing."
Each of these behaviors ends up strengthening the original belief. If you stay silent, your brain concludes, "See? I avoided sounding stupid. That was a close call." This makes the cycle even stronger the next time a similar situation comes up.
Becoming a Detective of Your Own Mind
The goal here isn't to force "positive thinking" or ignore your real concerns. It’s about becoming a detective of your own mind. CBT teaches you the skills to pause and investigate these automatic connections.
By learning to spot these thought-feeling-behavior cycles as they happen, you gain the power to intervene. You create a space between the trigger and your reaction, giving you a chance to choose a different path.
You start asking yourself some critical questions:
- Is this thought 100% true?
- What's a more balanced or realistic way to look at this?
- What action could I take that would challenge this belief instead of just confirming it?
This process is what we call cognitive restructuring. It's not about pretending the presentation isn't nerve-wracking. It's about shifting the narrative from "I will fail" to "This is challenging, but I am prepared, and I can handle it."
This more balanced thought leads to calmer feelings, which in turn supports more confident and effective behavior. By changing just one corner of the triangle, you can change the entire outcome.
Practical CBT Techniques You Can Use
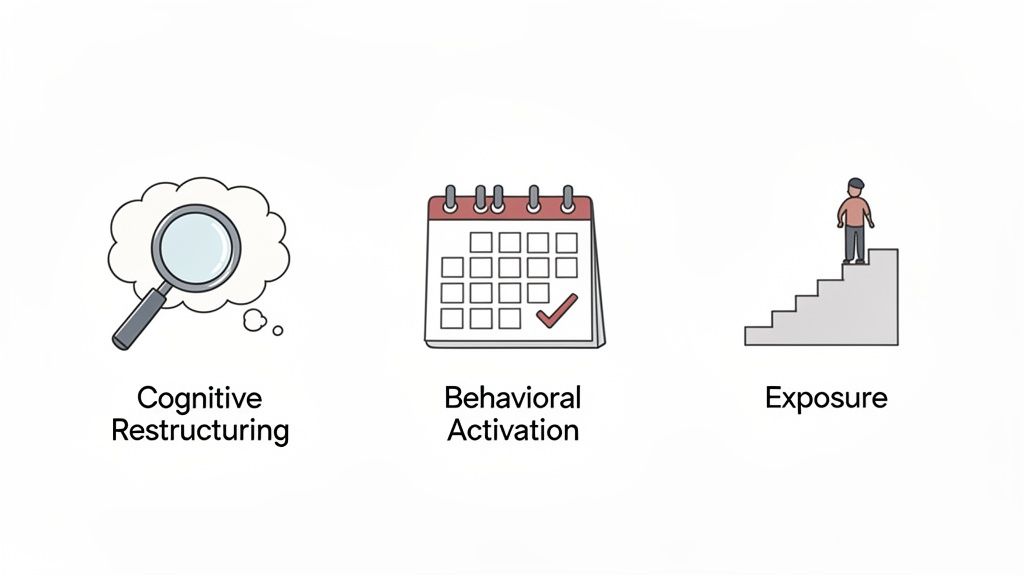
Knowing about the thought-feeling-behavior triangle is one thing; learning how to step in and change the pattern is where the real work begins. CBT isn't just a theory—it's a toolbox filled with practical, hands-on strategies designed to help you break out of unhelpful cycles.
Think of these techniques as exercises for your mind. Just as physical workouts build muscle, these mental exercises build resilience, emotional balance, and flexibility. Let's dig into three of the most powerful and widely used tools in the CBT toolkit.
Cognitive Restructuring: Challenging Your Automatic Thoughts
Cognitive restructuring is all about learning to question the unhelpful thought patterns that fuel so much of our distress. It's about becoming a detective for your own mind, learning to investigate your automatic thoughts instead of just accepting them as fact.
Many of these thoughts fall into predictable traps called cognitive distortions—they're like mental shortcuts that twist our perception of reality.
Some common cognitive distortions include:
- All-or-Nothing Thinking: Seeing things in black-and-white. If something isn’t perfect, you see it as a total failure.
- Mind Reading: Believing you know what others are thinking without having any real evidence.
- Catastrophizing: Automatically expecting the worst-case scenario and blowing negative possibilities way out of proportion.
- Fortune Telling: Predicting a negative future and treating that prediction as if it's already happened.
The goal here is to learn to catch these thoughts in the act, examine the actual evidence, and build a more balanced, realistic perspective. A popular tool for this is the thought record, which is a worksheet that guides you through this process step-by-step. To get some hands-on practice, our CBT workbook PDF is a great resource that walks you through these exact exercises.
Behavioral Activation: Re-engaging with Your Life
When your mood is low or you're struggling with depression, it’s natural to pull back from activities you once enjoyed. Behavioral activation is a powerful technique designed to reverse that trend. It’s built on a simple but profound principle: your actions can change how you feel.
Instead of waiting around to feel motivated, behavioral activation encourages you to schedule meaningful or pleasurable activities into your week, no matter what your mood is telling you. This helps break the grip of inertia and avoidance.
The process is pretty straightforward:
- Identify Activities: Brainstorm things you used to enjoy or that give you a sense of accomplishment or connection, even if they feel out of reach right now.
- Schedule Them: Put them in your calendar like you would a doctor's appointment. Start small and with something manageable.
- Track Your Mood: Notice how you feel before, during, and after. You might be surprised to find that even a small action gives you a lift.
This technique is incredibly effective because it provides direct, personal proof that your behavior can influence your feelings. It’s a way to actively generate positive experiences instead of just waiting for your mood to get better on its own.
This gradual re-engagement rebuilds confidence and disrupts the cycle of withdrawal that keeps depression going. In fact, research has shown that for many people, its effects are on par with antidepressant medication.
Exposure Therapy: Facing Your Fears Safely
For anxiety disorders, phobias, and OCD, exposure therapy is a cornerstone of effective CBT. The idea is to gradually and systematically face the situations, objects, or thoughts you fear in a safe, controlled way. While avoiding our fears brings temporary relief, it actually makes the fear stronger in the long run.
Exposure therapy works by helping your brain unlearn the connection between a trigger and a fear response. It’s a process called habituation. When you stay in a feared situation without the bad thing happening, your anxiety naturally starts to come down on its own.
To do this, a therapist helps you create a fear ladder or exposure hierarchy—a ranked list of feared situations, from the least scary to the most.
For example, someone with a fear of public speaking might create this ladder:
- Step 1: Saying "hello" to a cashier.
- Step 2: Asking a question in a small group meeting.
- Step 3: Voicing an opinion during a team call.
- Step 4: Presenting for five minutes to two colleagues.
- Step 5: Giving a short presentation to a larger group.
You start at the bottom and work your way up, only moving to the next step once you feel you've mastered the one before it. This structured approach ensures you’re never totally overwhelmed, building confidence and proving to yourself that you can handle the anxiety.
Adapting CBT for Neurodivergent Minds
Standard Cognitive Behavioral Therapy is a powerful framework, but it's not a one-size-fits-all solution. For someone with ADHD, Autism, or both (AuDHD), a rigid, unmodified approach can easily miss the mark. It can feel like trying to fit a square peg into a round hole.
The unique wiring of neurodivergent brains calls for a more flexible, personalized, and affirming approach. This is where adapted CBT comes in. It’s not about changing who you are; it’s about making therapy work for your brain.
Instead of seeing neurodivergence as a deficit to be fixed, this approach honors it as a different way of processing the world. The goal is to provide practical tools that empower you to navigate challenges in a world that wasn't always built for you. Understanding the concept of neurodiversity is key here—it moves the conversation from "curing" to "supporting," which makes all the difference.
Tailoring Techniques for Neurodivergent Brains
A skilled therapist knows how to adapt core CBT techniques to align with the strengths and challenges common in neurodivergent individuals. This often means shifting away from abstract concepts and toward concrete, tangible strategies that click with different learning styles.
For example, executive function challenges—like trouble with planning, organization, and emotional regulation—are common with ADHD. Instead of just talking about these issues, an adapted CBT session might involve:
- Visual Aids: Using whiteboards, charts, and diagrams to literally map out the thought-feeling-behavior triangle so you can see the connections.
- Breaking Down Goals: Deconstructing big, overwhelming tasks into tiny, manageable micro-steps to beat that feeling of paralysis and start building momentum.
- Integrating Special Interests: Weaving a client’s passions—whether it's video games, ancient history, or art—into therapy examples. This boosts engagement and helps the concepts stick.
A core principle of this adapted approach is recognizing that "can't" is often just a matter of "don't know how yet." The therapist's job is to co-create systems and strategies that bridge that gap, building skills rather than just demanding change.
This hands-on, skill-building focus makes adapted CBT a powerful tool for navigating common hurdles like Rejection Sensitivity Dysphoria (RSD), social communication difficulties, and managing emotional intensity.
A Strengths-Based and Affirming Model
Most importantly, this adaptation is done through a neurodiversity-affirming lens. This means your therapist understands and respects that neurodivergent traits are inherent, not flaws. You can learn more about what this looks like in practice by exploring our guide on neurodiversity-affirming therapy.
The work is centered on building self-awareness and self-compassion, helping you understand why your brain works the way it does.
For neurodivergent individuals, CBT becomes a skills-based intervention tailored to executive function, emotional regulation, and social communication. Globally, ADHD is estimated to affect around 5% of children and about 2.5–3% of adults, while Autism Spectrum Disorder affects roughly 1–2% of the population. This makes structured, scalable treatments essential.
Ultimately, adapting CBT for neurodivergent minds means meeting the client exactly where they are. It’s a collaborative process that builds on individual strengths, validates personal experiences, and provides customized tools for thriving.
Navigating Your First CBT Session via Telehealth
Stepping into therapy for the first time can feel like a big deal, especially when you’re not sure what to expect. Let's pull back the curtain on what a Cognitive Behavioral Therapy session actually looks like, particularly in a telehealth setting. The predictable, structured nature of CBT often comes as a huge relief, especially for neurodivergent individuals who thrive on clarity and routine.
Your first session is all about connection and gathering information. You'll meet your therapist, talk about what brought you in, and start outlining some initial goals. Think of it less like an interrogation and more like a collaborative strategy meeting where you and your therapist start sketching out a map together.
The Structure of a Typical Session
Most CBT sessions follow a clear, predictable pattern. This isn’t about sticking to a rigid script, but rather using a reliable framework to make sure every meeting is productive and keeps you moving forward.
A typical session usually flows like this:
- Check-in and Mood Review: You’ll start by touching base on your week, your overall mood, and anything significant that happened.
- Agenda Setting: You and your therapist will decide on a clear agenda for the session, agreeing on what specific topics or skills to focus on that day.
- Review of Homework: You'll go over any practices you tried between sessions, like a thought record, and discuss what you learned from the experience.
- Learning a New Skill: This is the core of the session, where you’ll learn and practice a new CBT technique.
- Wrap-up and New Practice: To close, you'll summarize the key takeaways and decide on a new practice to try before you meet again.
Making CBT Work Online
The rise of telehealth has made high-quality therapy more accessible than ever before. Online CBT sessions have the same structured, collaborative feel as in-person meetings, just with the added convenience of being at home. Instead of a physical whiteboard, your therapist might use a digital one to map out a cognitive triangle. Worksheets and thought records can be shared and filled out together in real-time, right on your screen.
The core of what is cognitive behavioral therapy—its structure, skill-building focus, and collaborative nature—translates seamlessly to a virtual environment. For many, getting support from the comfort of their own space removes major barriers and makes the whole process feel more manageable.
This accessibility is a huge reason for its worldwide growth. Beyond being clinically effective, CBT is a major health service. The global CBT market was valued between USD 7.63 and 7.81 billion in 2024, and it's projected to climb as high as USD 38.41 billion by 2035. North America is leading the charge, thanks to high mental health awareness and the widespread adoption of teletherapy. To see more on this trend, you can discover more insights about the CBT market on snsinsider.com.
This virtual format is especially helpful for those managing specific conditions from home. For families and individuals navigating ADHD, understanding how to make virtual care work is key. You can find more practical advice in our guide to online ADHD therapy that works. This approach ensures you get expert support without the added stress of travel, making it that much easier to build lasting skills for a more balanced life.
How to Find the Right CBT Therapist
Finding the right therapist isn't just a step in the process—it's one of the most important parts of your entire CBT journey. The connection and trust you build with your provider can make all the difference in your progress. You're looking for someone with the right credentials, yes, but also someone who truly gets you and your unique needs.
Think of it less like a search for a doctor and more like finding a partner for your mental health. A good therapist's office will often run smoothly, which can be a sign of their dedication to client care. Some even use a virtual assistant for therapy practice to handle the admin side so they can focus entirely on you.
Key Questions to Ask a Potential Therapist
Before you commit, it's smart to have a quick chat or consultation. This is your chance to see if they're the right fit for you or your child, especially when neurodivergence is part of the picture.
Here are a few questions you might want to ask:
- Credentials and Licensing: "Are you a licensed therapist, psychologist, or social worker in my state?"
- Specialized Experience: "What's your experience using CBT with clients who have ADHD and/or Autism?"
- Therapeutic Approach: "How do you adapt CBT for neurodivergent clients? Can you give me an example?"
- Affirming Practices: "How do you make sure your practice is neurodiversity-affirming?"
That last question is absolutely essential. A genuinely neurodiversity-affirming therapist won't see your brain's unique wiring as a "problem" to be fixed. They'll understand and validate experiences like masking in women and girls, viewing them as adaptations, not deficits.
Finding a therapist who sees and honors your unique brain wiring is non-negotiable. The right professional will empower you with tools that fit your life, not try to force you into a mold that doesn't fit your brain.
The Path to Clarity: A Diagnostic Evaluation
For many people, the journey doesn't start with therapy but one step before it: a diagnostic evaluation. This isn't about getting a label. It’s about getting clarity—a deep, meaningful understanding of your cognitive and emotional landscape.
An accurate diagnosis acts like a roadmap. It guides your therapist in choosing the most effective CBT strategies tailored specifically to you. This is the step that connects you to true, targeted well-being. At the Sachs Center, we see a diagnostic evaluation as the definitive path to understanding and support, empowering you to move forward with confidence and a clear plan.
Your CBT Questions, Answered
It’s completely normal to have questions when you’re thinking about starting therapy. If you're wondering what Cognitive Behavioral Therapy is all about and whether it could be the right path for you, you’re in the right place. Here are some clear, straightforward answers to the questions we hear most often.
How Long Does CBT Take to Work?
One of the great things about CBT is that it’s designed to be a shorter-term, goal-focused therapy. A typical round of CBT usually lands somewhere between 8 and 20 sessions, but that timeline is always adjusted to fit your specific needs and what you want to achieve.
Many people start to feel a positive shift within just the first few meetings. This isn't about finding a magic, instant cure. It’s about immediately starting to learn and use practical skills that can make a real difference in your day-to-day life. The whole idea is to build momentum right from the start.
Is CBT Effective for Children and Teenagers?
Absolutely. CBT is a well-researched approach that’s not only effective but also highly adaptable for younger clients. The key is that a good therapist doesn't use a one-size-fits-all model. They get creative, translating the core ideas of CBT into formats that are engaging and make sense for kids and teens.
For younger clients, this could look like:
- Using games and art projects to explore the link between thoughts and feelings.
- Creating stories or comics to show how to challenge those pesky, unhelpful thoughts.
- Setting up reward systems to help with the frustration and task avoidance that can come with ADHD.
This creative approach helps kids and teens learn vital skills for handling anxiety, navigating social situations, and managing their emotions in a way that feels empowering, not clinical.
How Is CBT Different from Other Therapies?
While many types of therapy can offer valuable insights, CBT stands apart because of its structure and focus. Unlike some traditional talk therapies that might spend a lot of time digging into your past to find the roots of your problems, CBT is primarily focused on the here-and-now and is forward-looking.
The real mission of CBT isn’t just to understand your challenges—it's to give you a practical, hands-on toolkit of skills you can actually use. It’s an active, collaborative process designed to build resilience that sticks with you long after therapy is over.
Do I Need a Formal Diagnosis for CBT?
Not always. Many people come to CBT to work on specific issues that don’t necessarily need a formal diagnosis, like figuring out how to stop procrastinating, building self-esteem, or getting over a particular fear. The skills you learn are useful for anyone who wants to improve their mental well-being.
That said, a formal diagnostic evaluation can be incredibly helpful. For conditions like ADHD or Autism, getting an accurate diagnosis allows your therapist to build a highly personalized and effective treatment plan that works with your unique brain wiring, not against it. It gives you both a clear roadmap for your journey.
At the Sachs Center, we specialize in providing that clarity through expert diagnostic evaluations for ADHD and Autism. Understanding your unique profile is the first step toward effective, personalized CBT. Learn more about our diagnostic and treatment services and book your evaluation today.