Is gene testing for ADHD a reliable way to get a diagnosis?
The short answer is no. While the science is fascinating and ADHD certainly has strong genetic roots, today’s genetic tests simply cannot diagnose ADHD or tell you with any certainty if you have it.
The Growing Interest in Gene Testing for ADHD
It’s completely natural to wish for a definitive, black-and-white test for Attention-Deficit/Hyperactivity Disorder (ADHD). For a condition that touches the lives of millions, the idea of a simple cheek swab providing clear answers is incredibly appealing for both parents and adults.
The goal of this guide is to untangle the scientific reality from the commercial promises. We'll give you a clear, honest look at where the technology actually stands today.
ADHD is one of the most common neurodevelopmental disorders out there. In fact, recent global analyses show it affects approximately 8.0% of children and adolescents. If you want to dive deeper into the numbers, a comprehensive 2023 review offers an extensive look at its prevalence worldwide.
This high prevalence, combined with a strong, well-established genetic link, is what really fuels the public’s curiosity. It's a logical question: if ADHD runs in families, shouldn't there be a gene test for it? This is exactly the line of thinking that leads many people to explore direct-to-consumer genetic testing.
The reality, however, is that the science is far more complex than a single test can capture.
Why a DNA Test Isn't a Diagnostic Tool
For anyone wrestling with their own symptoms, the search for answers can be all-consuming. But it's vital to start with a proper clinical evaluation, which remains the gold standard. You can learn more about the established diagnostic process by exploring our detailed guide on how to know if you have ADHD.
So why isn't a DNA test the answer? It’s because ADHD is what scientists call "polygenic." This means it isn’t caused by a single "ADHD gene" but is instead influenced by hundreds, maybe even thousands, of different genes. Each of these genes has only a tiny, subtle effect on its own.
Think of it like trying to predict a person's exact height. You know genetics play a huge role, but you can't look at one or two genes and know if they'll be 5'4" or 6'2". It’s the complex interplay of countless genetic factors, plus environmental influences, that determines the outcome. ADHD works in a similar way.
Current genetic tests can spot certain genetic markers that are associated with a slightly higher statistical risk, but they absolutely cannot predict or confirm the disorder. This is the crucial distinction we'll explore throughout this article.
To put it simply, here’s a quick snapshot of where things stand.
Current Status of Gene Testing for ADHD
| Aspect | Current Status |
|---|---|
| Diagnostic Use | Not approved or recommended for diagnosing ADHD. It cannot confirm or rule out the condition. |
| Scientific Basis | ADHD is highly heritable but polygenic—influenced by many genes with small individual effects. |
| Predictive Power | Very low. Tests can only identify a slightly increased statistical risk, not a definite outcome. |
| Clinical Standard | A comprehensive clinical evaluation by a qualified professional remains the only valid method for diagnosis. |
| Commercial Tests | Direct-to-consumer tests may provide interesting but not clinically actionable information about genetic predispositions. |
Understanding these limitations is key. It helps you focus on what truly matters for getting an accurate diagnosis and effective support: a thorough evaluation by an expert who understands the nuances of ADHD.
Understanding the Strong Genetic Roots of ADHD
To really get why gene testing for ADHD isn't straightforward, we first have to talk about the powerful role genetics play in the condition. Think of your DNA as a massive, complex recipe book for building a brain. Certain ingredients—your genes—don't automatically create a specific outcome, but they absolutely influence the final dish.
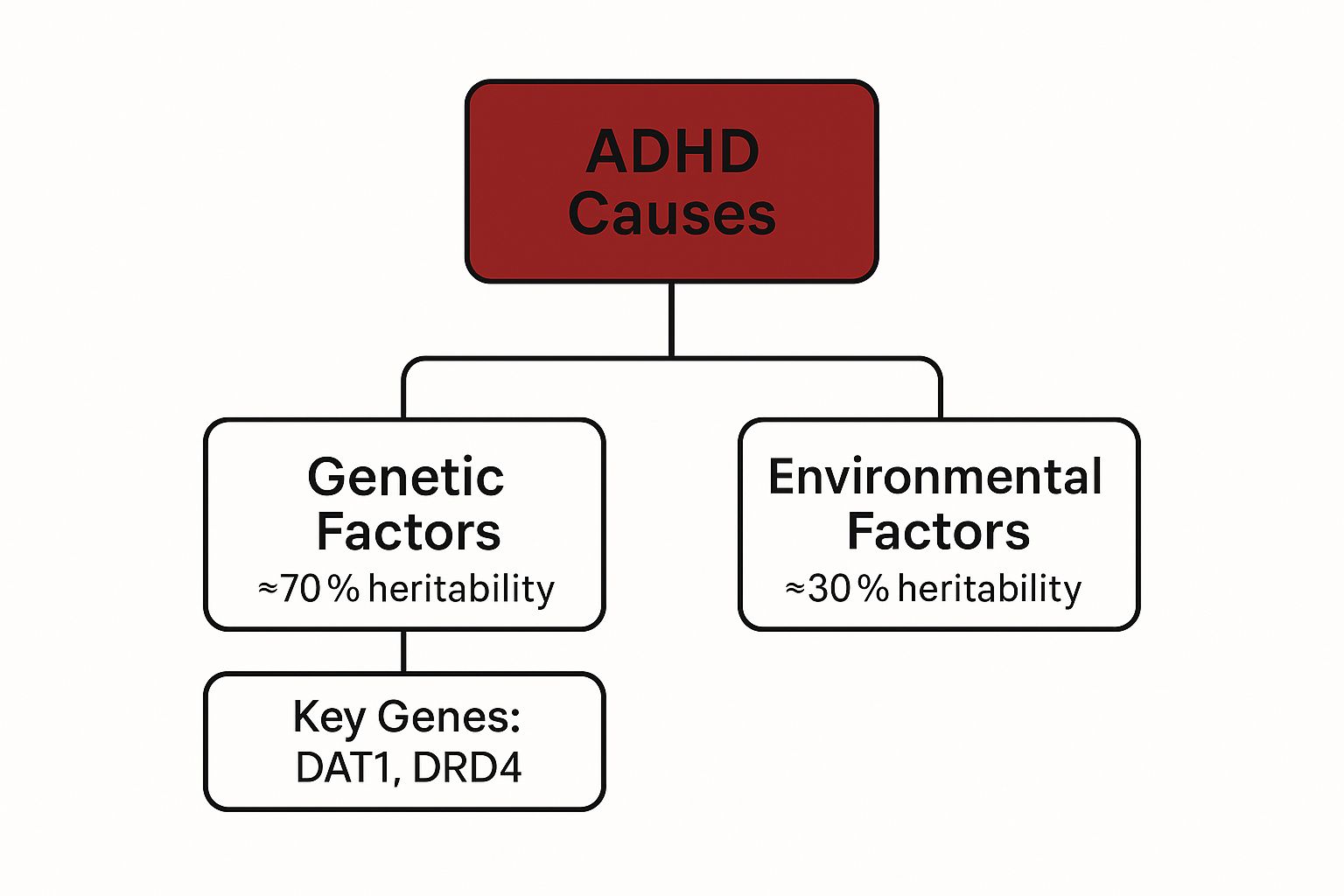
This idea is called heritability. For ADHD, genetics is a huge factor, with research estimating that between 70% to 80% of cases are tied to inherited genetic factors. This explains the strong familial risk and is a big reason why so many people are curious about genetic testing in the first place. You can dive deeper into the research on this powerful genetic link from Yale Medicine.
This infographic gives a clear visual breakdown of the primary factors contributing to ADHD, showing just how much weight genetics carries.
As you can see, environmental factors definitely play a part, but the genetic component is by far the biggest piece of the puzzle. It’s why ADHD so often runs in families.
Not a Single-Gene Disorder
It's really important to understand that ADHD isn't like a single-gene disorder, such as cystic fibrosis, where one specific faulty gene is the direct cause. In those cases, if a doctor finds that one problematic gene, the diagnosis is clear. That’s just not how it works with ADHD.
Instead, ADHD is a polygenic condition. This means its genetic risk is spread out across hundreds, maybe even thousands, of different genes.
A polygenic condition is like trying to predict a major storm. It isn't caused by just one thing, like wind speed. Instead, it’s the result of a complex mix of temperature, humidity, air pressure, and dozens of other variables all interacting at once. ADHD’s genetic roots work in a similar, multi-faceted way.
Each of these genes contributes only a tiny, subtle nudge toward the possibility of developing ADHD. No single gene holds the key.
The Role of Specific Genes
Over the years, researchers have pinpointed several genes that pop up more frequently in people with ADHD. Two of the most studied are:
- DAT1 (Dopamine Transporter Gene): This gene plays a role in how the brain transports dopamine, a key neurotransmitter involved in focus, motivation, and reward.
- DRD4 (Dopamine Receptor D4 Gene): This one helps build the receptors for dopamine, which influences how brain cells receive those crucial dopamine signals.
But here’s the catch: having a particular variant of these genes doesn't automatically mean you will have ADHD. Plenty of people have these common genetic variations and show no signs of the disorder.
This polygenic nature is precisely why gene testing for ADHD can’t give a simple yes-or-no diagnosis. For now, it remains a tool for research, not for clinical confirmation.
How Current Gene Tests for ADHD Actually Work
So, how do these tests actually peer into your DNA? It’s not as simple as finding one "ADHD gene." Instead, most direct-to-consumer companies use one of two main methods: genotyping or sequencing.
Think of your entire genome as a massive encyclopedia. Genotyping and sequencing are two very different ways of proofreading it, and understanding the difference is key to managing your expectations.
Genotyping: Spot-Checking for Common Markers
Genotyping is like giving a proofreader a specific list of known typos and telling them exactly which pages to check. They scan only those specific pages for those exact typos—they aren't reading the entire encyclopedia.
This method is fast and relatively inexpensive, which is why it's so common. In the context of ADHD gene testing, the test scans your DNA for specific, well-known Single Nucleotide Polymorphisms (SNPs). These are tiny, single-letter variations in your DNA that large population studies have statistically linked to a slightly higher risk of ADHD.
It’s crucial to understand that these tests are not looking for a definitive "ADHD gene." They simply identify a handful of these common markers, which are small risk indicators, not diagnostic certainties. For a reliable diagnosis, this information must be complemented by a comprehensive clinical evaluation. To see what that involves, you can review our guide on the complete ADHD testing process.
Sequencing: Reading the Full Story
Sequencing, on the other hand, is a much more thorough process. It’s like asking the proofreader to read an entire chapter—or even the whole book—word for word. This method can spot not only the known typos but also any rare or completely new ones that weren't on the original list.
While far more comprehensive, sequencing is also more expensive and complex. This is why it's less common in basic consumer tests and is primarily used in research to uncover new genetic links.
The most important takeaway is that neither genotyping nor sequencing can "diagnose" ADHD. Genotyping provides a narrow look at common risk markers, while sequencing offers a broader view that is better suited for research than for individual diagnosis at this time.
This more detailed approach is helping scientists explore other complex genetic factors, like de novo mutations—spontaneous genetic changes that are not inherited from parents. Though rare, these unique variants can significantly impact ADHD risk. In fact, cutting-edge research is now using DNA sequencing of families to find that some ADHD cases come from these spontaneous mutations. You can learn more about how researchers are identifying ADHD risk genes through these variants.
This just adds another layer of complexity, highlighting why a simple spit test can't capture the full, intricate genetic picture of ADHD.
Evaluating the Clinical Validity and Limitations
This brings us to the million-dollar question: do these genetic tests actually work for diagnosing ADHD? To get to the heart of it, we need to understand two very different ideas: analytical validity and clinical validity.
Analytical validity is simple. It asks, "Does the test accurately find the specific gene variant it's looking for?" For most modern genetic tests, the answer is a confident yes. They are very good at identifying the specific DNA sequences they’re designed to find.
But that’s only half the story. The much more important question for anyone considering a test is about clinical validity.
What Is Clinical Validity?
Clinical validity asks a tougher question: "Does finding that gene variant actually predict a specific health condition?"
Think of it like this. A smoke alarm has great analytical validity—it's excellent at detecting smoke. But if that same alarm goes off every single time you make toast, its clinical validity for predicting a house fire is terrible. It detects the marker (smoke) but can't reliably predict the condition (a fire).
When it comes to ADHD, the clinical validity of current genetic tests is, unfortunately, quite low. They can correctly identify certain gene markers, but those markers are surprisingly poor predictors of whether someone actually has or will develop ADHD.
A genetic test for ADHD might find a "risk" variant, but that's like finding a single lottery ticket in someone's pocket. It slightly increases their chance of winning, but it’s a very long way from guaranteeing they'll hit the jackpot. Most people with that "at-risk" ticket will never win, and many winners will have bought completely different tickets.
The Problem of Polygenic Risk Scores
To get around the fact that ADHD is linked to many, many genes, researchers came up with something called a Polygenic Risk Score (PRS). A PRS scoops up data from hundreds or even thousands of genetic markers associated with ADHD and boils it all down into a single score. The goal is to estimate a person's overall genetic likelihood of having the condition.
While this is an incredible tool for large-scale research studies, a PRS is simply not a diagnostic tool for an individual. It’s like a weather forecast that predicts a 20% chance of rain across your entire city. That's useful information for city planners preparing for potential flash floods, but it can’t tell you if it will rain on your specific street corner at 3 PM.
A PRS might place someone in a statistically higher risk group, but it falls far short of giving a clear "yes" or "no" for that person. There are a few big reasons for this:
- Tiny Effects: Each individual gene contributes only a tiny, almost insignificant fraction to the overall risk.
- Life Happens: A person’s environment—from their prenatal development to their home life and school experiences—plays a massive role that no genetic test can account for.
- Built on Averages: These scores are based on huge population averages, and they lose their accuracy when you try to apply them to just one person.
The bottom line is this: gene testing for ADHD can identify certain risk factors, but it absolutely cannot confirm or rule out the condition. The science just isn't there yet.
Weighing the Pros and Cons of ADHD Genetic Testing
After digging into the science, it's time to get practical. If you're thinking about gene testing for ADHD, it’s absolutely critical to weigh what you might gain against what you could lose. The reality is, the potential benefits are quite limited, while the drawbacks are very real and significant.
I get the appeal. A report that points to a higher genetic likelihood can feel incredibly validating. For someone who has struggled with symptoms for years, seeing that biological component in black and white can be the final push needed to seek a proper clinical evaluation. It's a form of personal confirmation.
But that's really where the good news stops. Right now, with the science as it is, the cons list is just a lot longer and heavier than the pros.
The Major Downsides of Today's Tests
The single biggest risk is misinterpretation. It's so easy to look at a "high-risk" result and see a diagnosis. It's not. It can't be. This misunderstanding can stir up a lot of unnecessary anxiety and create a false sense of certainty about a very complex condition.
Then there's the danger of genetic fatalism. This is the trap of thinking, "well, it's in my genes, so I'm stuck with it." This mindset is not only wrong, but it's also incredibly counterproductive. It can stop people from even trying the very things we know work—like therapy, coaching, and behavioral strategies that have been proven to help manage ADHD effectively.
A genetic test can't tell you about your resilience, your strengths, or your capacity to learn and adapt. Placing too much emphasis on genetic predispositions overlooks the powerful role that environment, support systems, and personal effort play in shaping your life's outcomes.
The bottom line is that the information from current ADHD genetic tests just isn't clinically actionable. Your doctor can't use it to diagnose you. They can't use it to prescribe a specific medication or create a targeted treatment plan. For now, it's interesting data for researchers, but it offers very little practical value for your personal health journey.
Weighing the Pros and Cons of Current ADHD Gene Tests
When you lay it all out, the picture becomes clearer. The potential for a small amount of validation comes with some serious risks that are important to consider.
| Potential Pros (Limited) | Significant Cons (Current Reality) |
|---|---|
| Personal Validation: Can confirm a long-held suspicion that challenges have a biological basis. | High Risk of Misinterpretation: "High-risk" results are often mistaken for a clinical diagnosis, causing undue stress. |
| Motivation for Evaluation: May encourage someone to finally seek a formal diagnosis from a qualified professional. | Genetic Fatalism: Can lead to a belief that one's fate is sealed, discouraging proven behavioral interventions. |
| Satisfies Curiosity: Provides a piece of the puzzle for those deeply interested in their genetic makeup. | Not Clinically Actionable: Doctors cannot use this data to diagnose, treat, or prescribe medication for ADHD. |
| Privacy & Data Risks: Sharing your DNA with commercial companies has long-term privacy implications. | |
| Financial Cost: These tests aren't cheap, and the cost doesn't align with the limited practical benefits. |
Ultimately, the decision is a personal one, but it should be an informed one. The science simply isn't there yet to make these tests a reliable or useful tool for individuals.
The Price of Curiosity and Your Privacy
Lastly, we can't ignore the very real privacy concerns. When you send your saliva sample to a direct-to-consumer testing company, you are handing over the most fundamental, personal data you have. The fine print on how that data is stored, shared, or even sold can be a maze, and these policies can change over time, putting your genetic privacy at risk in ways you might not anticipate.
So before you spend the money, ask yourself: are these very limited insights truly worth the cost, the potential for more anxiety, and the risk to your personal data? For most people, the answer right now is probably no.
The Future of Genetics in ADHD Diagnosis and Treatment
While today’s gene tests for ADHD can’t give us a definitive diagnosis, it’s a mistake to see this as a dead end. Instead, think of it as the very beginning of a much deeper journey into understanding the condition. The real goal of all this research isn't just about finding a label, but about tailoring treatment with incredible precision.
Massive research projects are underway, meticulously mapping the complex genetic landscape of ADHD. As scientists pore over the DNA of hundreds of thousands of people, they're slowly piecing together a more detailed "recipe" for the condition. This expanding knowledge is gradually clarifying which genetic pathways are the most influential.
A Shift Towards Personalized Treatment
The most exciting future for gene testing for ADHD isn’t actually about diagnosis at all. It’s in a field called pharmacogenomics—the science of using your personal genetic information to predict how you'll respond to specific medications.
Imagine a future where the trial-and-error process of finding the right medication is a thing of the past. Instead, a simple genetic test could help your doctor predict:
- Which ADHD medication is most likely to work for you.
- The ideal dosage to get the most benefit with the fewest side effects.
- Which medications to avoid because you have a higher risk of a bad reaction.
This would be a profound shift away from a one-size-fits-all approach to a truly personalized one. Understanding this genetic dimension is key, especially when dealing with the complexities of how conditions like ADHD and autism can show up together. For anyone navigating this, learning more about a combined ADHD and autism diagnosis can offer valuable context.
The ultimate vision for pharmacogenomics is to remove the guesswork from prescribing. It’s about using your unique genetic blueprint to find the right therapeutic match from the very beginning, improving outcomes and reducing the frustrating process of trying multiple medications.
It’s crucial to remember that this vision is still on the horizon. Although the research is active and incredibly promising, pharmacogenomic testing for ADHD isn't part of standard clinical practice yet. The future is bright, but for now, we must rely on today's proven methods for care.
Questions We Often Hear About ADHD Gene Testing
As you dive into the complex world of ADHD, it's completely normal to have questions, especially when it comes to new technologies like genetic testing. Let’s tackle some of the most common questions we hear, giving you straight answers based on where the science stands today.
Can a Gene Test Diagnose My Child's ADHD?
The short answer is no. A genetic test can't diagnose ADHD in a child or an adult.
While ADHD is highly heritable—meaning it definitely runs in families—it’s also a polygenic condition. Think of it like a puzzle with hundreds of tiny pieces. Each gene contributes just a tiny part of the overall picture. Current tests can’t put all those pieces together to give you the definitive “yes” or “no” that a full clinical evaluation can.
Right now, gene testing for ADHD is mostly valuable for researchers trying to understand the condition, not for diagnosing it in a clinic.
It's so important to understand this: a "high-risk" result from a genetic test is not a diagnosis. It’s just a statistical probability, and it doesn't have the clinical certainty needed to confirm ADHD in any single person.
Will a Genetic Test Tell Me Which ADHD Medication Is Best?
This is where things get exciting for the future, but we're not quite there yet. This field, called pharmacogenomics, is working to connect specific genes to medication responses. The goal is to one day predict which drugs will work best with the fewest side effects for a specific person.
For now, though, this isn't a standard part of clinical care. Finding the right medication still comes down to a doctor’s expertise and a patient's own experience, not a DNA test.
Is It Worth Getting a Genetic Test Just for My Own Information?
This is a personal call, but it’s crucial to weigh the very limited benefits against some significant drawbacks. Sure, a test might feel validating if it points to a biological reason for your struggles, but that validation comes with real risks.
- Easy to Misinterpret: It’s incredibly easy to see a "high-risk" result as a firm diagnosis, which can cause a lot of unnecessary anxiety.
- Privacy Concerns: You're handing over your most sensitive biological data to a commercial company. It's worth thinking about what that means for you.
- Not Actionable: The information you get can't actually be used by your doctor to guide your treatment plan.
For most people, the potential for confusion and the privacy risks just don't stack up against the benefit of satisfying personal curiosity.
At the Sachs Center, we are committed to using proven, evidence-based methods for accurate diagnosis and effective treatment. While the future of genetics is promising, today's gold standard is still a thorough, compassionate clinical evaluation. If you're looking for clarity for yourself or a loved one, we offer comprehensive virtual assessments for ADHD, Autism, and AuDHD. Learn more about our diagnostic evaluations and take the next step.