If bedtime feels more like a battle than a gentle winding down, you’re in the same boat as countless other parents. Many kids with ADHD really struggle with sleep, but it’s not a behavioral issue—it’s often because their brain’s internal clock is on a completely different schedule. In fact, a staggering up to 75% of children with ADHD face significant sleep problems, which can turn a simple nightly routine into a major source of stress for the whole family.
The ADHD Brain and The Struggle with Sleep

For parents of kids with ADHD, calling bedtime a "battle" often feels like an understatement. It can be a draining, frustrating cycle that leaves everyone feeling worn out. But what if the resistance isn't about defiance? What if it’s a direct reflection of your child’s unique brain wiring? Grasping this connection is the first real step toward finding solutions that actually work.
Imagine the ADHD brain as a high-performance engine that just doesn't know how to idle. As evening sets in and other kids' minds naturally start to power down, the ADHD brain often stays in high gear. This makes the transition from being awake and alert to calm and sleepy incredibly challenging. It's not a choice; it's just how their brain operates.
Why Sleep Doesn't Come Easily
So, what's really going on here? Several core features of ADHD create the perfect storm for bedtime troubles. It’s a mix of biology and environmental triggers that can make falling asleep feel next to impossible. For a deeper dive, you can explore the common sleep problems associated with ADHD and how they show up.
The main reasons behind these sleep issues usually boil down to a few key things:
- Delayed Circadian Rhythm: Think of this as the body's internal clock. In many children with ADHD, this clock is set later. Their brains don't start producing melatonin—the hormone that says, "Hey, it's time to sleep!"—until much later at night, sometimes hours after their peers.
- Hyperactivity and Racing Thoughts: That classic hyperactivity doesn't just switch off when the lights go out. For many kids, it turns into a physically restless body and a mind that won’t stop spinning with ideas, daydreams, or worries. Settling down feels like trying to stop a merry-go-round at full speed.
- Sensory Sensitivity: Kids with ADHD often experience the world more intensely. A scratchy tag on their pajamas, a faint sound from downstairs, or a tiny sliver of light under the door can feel like a major distraction, pulling them right out of a sleepy state.
At its heart, the problem is often a biological mismatch. Your child’s brain is simply on a different schedule than the rest of the world. This creates a constant tug-of-war between when they should be sleeping and when their body is actually ready to sleep.
The Role of Stimulant Medications
Adding another layer to this puzzle, the stimulant medications frequently used to manage ADHD symptoms can also disrupt sleep. While these medications are a huge help for focus and impulsivity during the school day, their effects can sometimes linger into the evening hours.
This creates a real Catch-22 for parents and doctors. The very medication that helps a child thrive during the day might be part of the reason they can't fall asleep at night. It’s a common dilemma and underscores why it’s so important to work closely with your child’s doctor. Fine-tuning medication and understanding this interplay between the ADHD brain and sleep is crucial before considering any sleep aids.
How Melatonin Tells the Brain It's Time for Sleep
It’s easy to think of melatonin as a sedative, like a sleeping pill that just knocks you out. But that’s not really how it works. A better way to think of it is as the body's own personal sunset. It's a gentle signal to the brain that darkness has fallen and it's time to start winding down for the night.
Melatonin is the starting pistol for sleep, not the finish line. It doesn't force your child's brain to shut down. Instead, it creates the perfect conditions for sleep to happen naturally. Getting this distinction right is key to using melatonin for kids with ADHD effectively.
The Hormone of Darkness
There’s a good reason scientists often call melatonin the “hormone of darkness.” Its production is directly tied to light. When your child’s eyes detect fading light at the end of the day, a tiny, pinecone-shaped gland in the brain—the pineal gland—gets the cue to start producing and releasing melatonin.
As those melatonin levels rise, the hormone travels through the bloodstream and binds to special receptors in the brain. This kicks off a chain reaction: body temperature drops slightly, alertness fades, and a feeling of drowsiness begins to set in. It’s less like flicking a switch and more like slowly dimming the lights, preparing the body for rest.
Melatonin is a timing hormone, not a knockout drug. Its main job is to set the body's internal 24-hour clock, or circadian rhythm, by signaling that it's time to sleep.
For many children with ADHD, this whole process is delayed. Their brains might not start releasing melatonin until much later in the evening, which is a big reason why they can feel so wide-awake and restless long after their bedtime.
The ADHD-Melatonin Link
The connection between ADHD and a delayed sleep cycle isn't just a behavioral quirk; it's rooted in biology. The internal clocks of many kids with ADHD seem to run on a different schedule, making it genuinely difficult for them to feel tired at a "normal" bedtime.
Research is digging deeper into why this happens. One fascinating genetic study on nature.com found that children with specific gene variations that led to lower nighttime melatonin levels also tended to have more severe ADHD symptoms. This suggests melatonin doesn't just influence sleep—it might also play a role in the core brain functions affected by ADHD.
Animal studies back this up, showing that melatonin helps regulate dopamine and noradrenaline, two key brain chemicals that are often out of balance in ADHD.
This all points to a critical takeaway for parents: the sleep problems aren't just a symptom of ADHD; they're woven into the very fabric of the condition. When you give supplemental melatonin, you're essentially providing that missing "it's nighttime" signal a bit earlier, helping to nudge your child’s internal clock back into sync.
Finding the Right Melatonin Dose and Timing
Once you and your child's pediatrician have decided to give melatonin a try, the next big question is: how much, and when? Nailing the dose and timing is what makes melatonin a helpful tool instead of just another thing you've tried. This isn't about finding a single magic number; it's about a personalized approach tailored to your child's specific sleep struggles.
The golden rule here is simple: start low and go slow. This is not a race. The real goal is to find the smallest effective dose—just enough to help your child wind down and fall asleep without waking up groggy the next morning.
The "Start Low and Go Slow" Approach
For most kids, this journey begins with a tiny dose, often between 0.5 mg and 1 mg. It might seem minuscule compared to the big bottles you see on pharmacy shelves, but children are far more sensitive to melatonin's effects. Starting small allows you to see how their body responds and adjust gently, always with your doctor's input.
This careful, step-by-step process is crucial. It helps you avoid giving too much, which can sometimes backfire and cause side effects like intense dreams or even waking up during the night. Think of it as giving the brain a gentle nudge, not a hard shove, toward sleep.
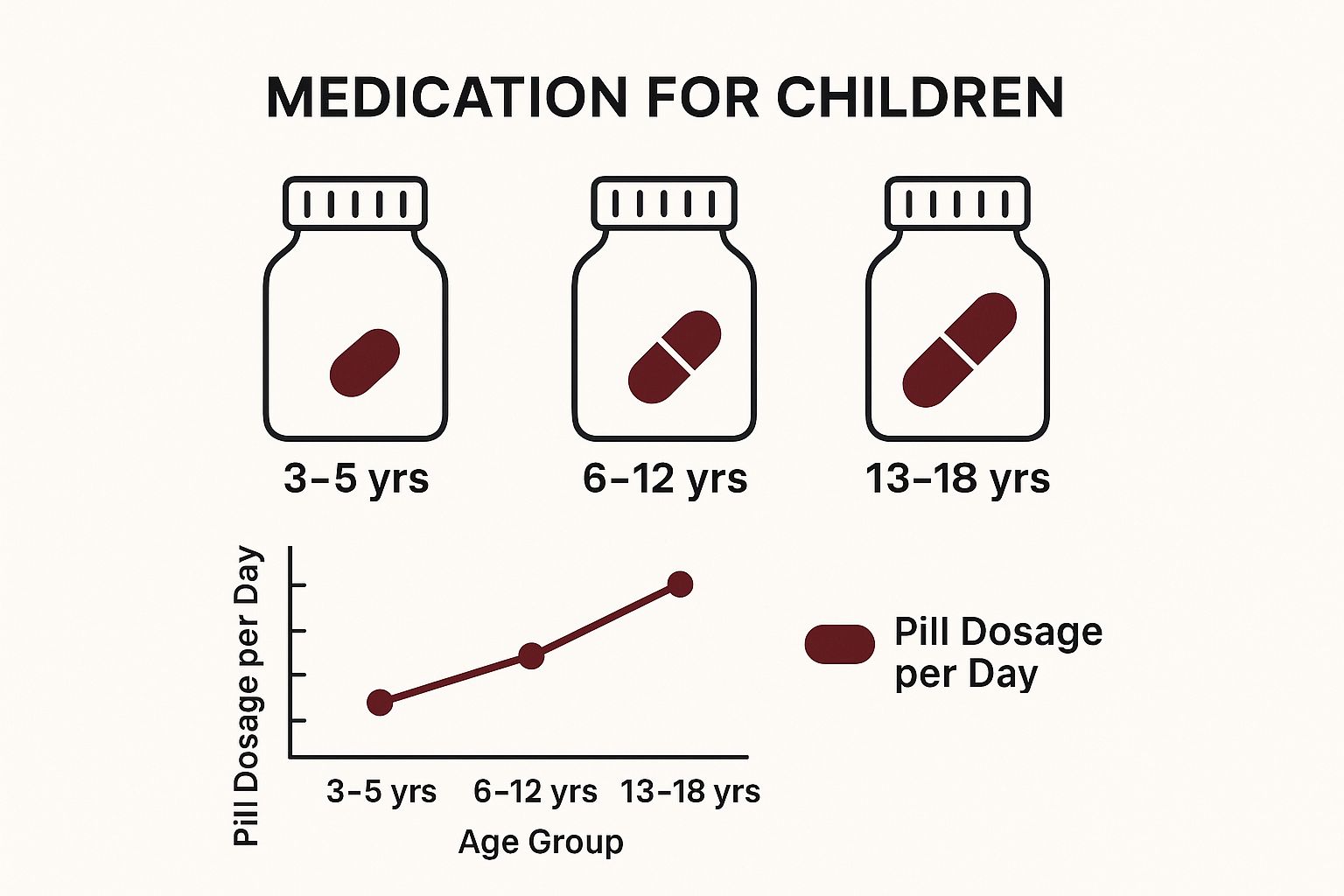
The image below gives a general idea of the starting dose ranges pediatricians often consider for different age groups.
As you can see, dosing isn't one-size-fits-all. It’s a decision that needs to be made thoughtfully, based on age and a doctor’s guidance.
Why Timing Is Everything
The "when" is just as important as the "how much." Melatonin is a timing hormone, so its power lies in giving it at the right moment to help reset your child's delayed internal clock. Give it too early or too late, and you might not see any effect—or you could accidentally shift their sleep cycle in the wrong direction.
The sweet spot for most kids is 30 to 90 minutes before their target bedtime. This gives the supplement enough time to get absorbed and for melatonin levels to rise in the bloodstream, sending that all-important "it's time for sleep" signal to the brain. So, if bedtime is 8:30 PM, you'd give the dose sometime between 7:00 PM and 8:00 PM.
The goal is to align the rise in melatonin with the beginning of the natural "sleep gate"—that window of time when the body is most receptive to falling asleep. This helps the brain learn a new, earlier bedtime.
The American Academy of Pediatrics (AAP) acknowledges that many children with ADHD respond well to carefully supervised doses between 0.5 mg and 6 mg, taken 30 to 90 minutes before bed. However, they also stress that long-term effects on development aren't fully known, which is exactly why having a pediatrician in your corner is non-negotiable.
To simplify, here are the core guidelines to discuss with your doctor.
Melatonin Dosing and Timing Guidelines for Children with ADHD
This table provides general starting points for melatonin dosage and timing for discussion with a pediatrician. It is not a substitute for medical advice.
| Guideline | Recommended Approach | Explanation |
|---|---|---|
| Starting Dose | Begin with 0.5 mg to 1 mg. | This minimal dose helps assess your child's sensitivity and avoids unnecessary side effects. |
| Timing | Administer 30 to 90 minutes before bedtime. | This window allows melatonin levels to peak just as your child is getting into bed, signaling that it's time for sleep. |
| Adjustment | Increase dose only if needed and under medical supervision. | Changes should be made slowly, in small increments (e.g., adding 0.5 mg), to find the lowest effective amount. |
| Consistency | Give melatonin at the same time every night. | This reinforces a consistent sleep-wake cycle, which is crucial for children with ADHD. |
Remember, these are just starting points. Every child is different, and finding the right formula often takes a little bit of patient trial and error with your doctor's help.
Choosing the Right Form for Your Child
Finally, you have to get your child to actually take it! Luckily, melatonin comes in a few different kid-friendly forms. The best one for you will depend on your child's age, sensory preferences, and whether they can swallow pills.
- Liquids: Perfect for younger kids or those who struggle with solids. A dropper allows for super-precise dosing, which is great when you're starting with tiny amounts.
- Chewables: A popular choice that often comes in pleasant flavors. Just be sure to check the label for allergens or extra sugar you don't want.
- Gummies: These are often the easiest sell because they feel like a treat. Again, keep an eye on the sugar content and other ingredients.
- Pills/Capsules: Best for older kids and teens who have no problem swallowing pills. This form often provides a wider variety of dosage strengths.
Working hand-in-hand with your pediatrician to dial in the right dose, timing, and form is the surest way to successfully use melatonin for kids with ADHD and help everyone in the family get a better night's sleep.
Navigating Safety Concerns and Side Effects
When you're thinking about giving your child any supplement, safety is always the first thing on your mind. So, let’s talk about that. The good news is that for short-term use, melatonin is generally considered safe and well-tolerated by most kids and teens. It's actually one of the most studied sleep aids for children, but "generally safe" doesn't mean there's nothing to keep an eye on.
Knowing the potential side effects helps you know what to watch for and gives you the right questions to ask your doctor. Most of these are mild and usually go away on their own or with a simple tweak to the dosage.
Common but Mild Side Effects to Monitor
Most side effects tied to melatonin are pretty minor, but it's still important to recognize them. The most common one by far is morning grogginess—that "hungover" feeling some kids get. This is almost always a sign that the dose was a little too high or given a bit too late the night before, so its effects are still lingering when the alarm clock goes off.
Here are a few other things you might see:
- Dizziness or Headaches: Some kids might feel a bit dizzy or get a mild headache, which usually fades as their body gets used to the supplement.
- Vivid Dreams or Nightmares: You might hear about more intense or memorable dreams, which can happen when melatonin influences sleep cycles.
- Increased Bedwetting: It’s less common, but some parents have reported an increase in bedwetting (nocturnal enuresis).
- Nausea: A small number of children might complain of an upset stomach after taking it.
It's also worth remembering that some of these can overlap with other things. For example, if your child is taking stimulant medication, it can be helpful to understand common ADHD medication side effects to help sort out what might be causing what.
The Big Question: Long-Term Safety and Puberty
The biggest point of caution when using melatonin for kids with ADHD centers on long-term use. Melatonin isn't just a sleep aid; it's a hormone. Because of that, there are real questions—and some theoretical concerns—about how using it for long stretches could affect a child's own hormonal development, especially around puberty.
The heart of the matter is a lack of long-term research. We simply don't have definitive studies that have followed kids taking melatonin for years, all the way through their teenage development. This knowledge gap is why experts urge parents to be cautious and always work with a doctor.
This isn't to scare you, but to give you the full picture. The goal should be to use melatonin as a temporary tool to get a healthy sleep cycle back on track, not as a permanent nightly fix. Your pediatrician will likely suggest taking breaks from it now and then—sometimes called "melatonin holidays"—to see if your child can maintain that new sleep schedule on their own.
The Supplement Problem: Dosage and Purity
Here's another crucial safety issue that catches many parents by surprise. In the United States, melatonin is sold as a dietary supplement, not a prescription drug. This detail has huge implications. The FDA (U.S. Food and Drug Administration) doesn't regulate supplements for purity or dosage accuracy nearly as strictly as it does for medications.
What does that actually mean for you when you're standing in the pharmacy aisle?
- Wildly Inaccurate Dosing: Research has shown that the amount of melatonin in a bottle can be completely different from what the label says. One major study found that some products contained over 400% more melatonin than advertised. Others had much less.
- Unlisted—and Concerning—Ingredients: That same study made another shocking discovery: 26% of the supplements they tested contained serotonin, another powerful hormone that was not listed on the label at all.
To get around this, you have to be a savvy shopper. Stick with reputable brands that have their products tested by an independent third party. Look for a seal on the label from organizations like USP (U.S. Pharmacopeia) or NSF International. This seal is your best bet for an extra layer of assurance that what's in the bottle actually matches what's on the label. Doing this homework is a non-negotiable part of using melatonin safely and responsibly for your child.
What the Science Says About Melatonin for ADHD
When you're trying to make the best decisions for your child, it helps to look past anecdotes and see what the actual data shows. So, what does the research say about giving melatonin to kids with ADHD? The scientific community has been looking into this for a while, and the evidence is pretty clear on one major point: it really helps with the frustrating, drawn-out process of falling asleep.
Most of the clinical studies have focused on something called sleep onset latency. That’s just the technical term for how long it takes to drift off after you turn out the lights. For a child with ADHD, this can feel like an eternity—an hour or more of tossing, turning, and a brain that just won't switch off. This is precisely where melatonin shines.
Getting to Sleep Faster
Study after study has shown that melatonin can significantly cut down the time it takes for a child with ADHD to fall asleep. We're not talking about a few minutes here and there. On average, research finds that it helps kids doze off 20 to 50 minutes faster.
That might not sound like a miracle, but for a parent who’s used to a two-hour bedtime battle, getting back nearly an hour of their evening is a massive win. It’s a game-changer for the whole family's peace and sanity.
This benefit is even more noticeable in kids who take stimulant medication. Those medications are great for daytime focus, but they can sometimes make it harder for the body to wind down at night. Melatonin essentially steps in to provide that gentle "sunset signal" the brain needs to start the sleep cycle, helping to counteract the lingering effects of the stimulant.
The big takeaway from all the research is this: Melatonin is a reliable way to help a child with ADHD fall asleep more quickly. It helps reset that delayed internal clock that's causing all the bedtime friction in the first place.
Adding More Overall Sleep Time
Of course, falling asleep is only half the battle. Staying asleep long enough is just as important for a child’s mood, learning, and ability to manage their symptoms. The good news is that the research also shows melatonin can increase total sleep time, though the gains here are usually a bit more modest.
For instance, one study looked at kids and teens with ADHD who were on stimulant medication. When they were given a small 1 mg dose of melatonin, their total sleep time went up by an average of 22 extra minutes a night. That might not sound like a lot, but it adds up to almost three extra hours of restorative rest every single week. You can read the full research about these findings on PMC to see for yourself how even a tiny dose can make a real difference.
That extra sleep gives the brain more time to recharge, which is crucial for handling the challenges of the next day.
What the Research Still Doesn't Tell Us
It’s just as important to be honest about what we don't know yet. While the evidence for short-term use is very solid, most studies have been on the shorter side—usually a few weeks or months. We definitely need more long-term research to see what the effects look like over several years, especially as kids go through puberty and major hormonal changes.
Another thing to keep in mind is that melatonin is a "sleep starter," not necessarily a "sleep sustainer." While it’s fantastic at helping kids fall asleep, its effect on staying asleep (what researchers call sleep efficiency) is less predictable. Some studies find it helps reduce waking up in the middle of the night, but others show little to no impact.
Knowing both the strengths and the current gaps in the research allows you to have a much more productive conversation with your child's doctor. It helps you work together to use this tool in the smartest, safest way possible.
Building a Healthy Sleep Routine Beyond Melatonin
While melatonin can feel like a game-changer for kids with ADHD, it’s really just one piece of the puzzle. The best way to think of it is as a temporary support—like training wheels on a bike. It helps your child get moving in the right direction, but the ultimate goal is for them to ride confidently on their own.
That independent ride comes from rock-solid sleep hygiene. A calm, predictable environment is the most powerful signal you can send to your child’s brain that it's time to wind down. This approach works with their biology, not against it, helping to naturally reset their internal clock over time.
The Power of a Predictable Bedtime Routine
For a child with an ADHD brain, which craves structure and predictability, a consistent bedtime routine is absolutely essential. The repetition acts as a series of signposts, guiding their active mind and body toward rest. It's less about just checking boxes and more about creating a runway for sleep.
Beyond just using melatonin, establishing an effective bedtime routine is what creates lasting change. The secret is to keep it calming and predictable, gradually shifting from more stimulating activities to quieter ones as bedtime draws near.
A simple but effective routine might look like this:
- Warm Bath or Shower: The slight drop in body temperature after a warm bath is a natural cue for sleepiness.
- Quiet Time: This is the time to put away screens. Instead, try reading a book together, listening to mellow music, or working on a simple puzzle.
- Final Connection: Spend a few minutes just talking quietly, giving a gentle back rub, or telling a story. This can help soothe any end-of-day worries.
Creating the Ideal Sleep Environment
The bedroom itself has a huge impact on sleep quality. Your mission is to turn it into a cave: cool, dark, and quiet. This minimizes the sensory input that can easily distract a sensitive ADHD brain.
Try to see the room through your child's eyes. That tiny blinking light on a charger or the muffled sound of a TV downstairs can feel like a spotlight in a dark theater when they're trying to drift off. Even small tweaks can make a massive difference.
Your child's bedroom should be a sanctuary for sleep and nothing else. When the brain starts to associate the bed only with rest, making that transition each night gets so much easier.
You can get started tonight by implementing some of these essential tips for a good night's sleep.
Critical Lifestyle Adjustments for Better Sleep
A few key habits throughout the day can set the stage for a successful night. These adjustments help regulate your child’s internal clock and remove common roadblocks to sleep.
-
Enforce a Strict Screen Curfew: The blue light from phones, tablets, and TVs is notorious for disrupting sleep because it actively suppresses the brain's own melatonin production. Set a firm family rule: all screens off at least 60-90 minutes before bed. No exceptions.
-
Watch for Hidden Caffeine: We all know to avoid soda before bed, but caffeine is sneaky. It can hide in iced tea, some "healthy" energy waters, and even chocolate. That piece of chocolate cake after dinner might be just enough to keep an ADHD brain buzzing for hours.
-
Get Morning Sunlight: This is one of the most powerful ways to anchor the body's clock. Just opening the blinds wide or spending a few minutes outside right after waking up sends a strong signal to the brain that it’s time to be alert, which helps regulate the entire 24-hour cycle.
By weaving these foundational habits into your daily life—along with the targeted support of melatonin under a doctor's guidance—you’re creating a comprehensive strategy. This approach doesn't just solve the immediate problem of falling asleep; it builds the skills and routines needed for a lifetime of better rest.
Your Questions, Answered
Deciding to give your child any new supplement is a big step, and it's natural to have questions. Let's tackle some of the most common concerns parents have when considering melatonin for their child with ADHD.
Is Melatonin Addictive for Children?
This is probably the number one question parents ask, and for good reason. The short answer is no, melatonin is not physically addictive like prescription sleep aids. Your child’s body won't become dependent on it to function.
That said, it's possible to develop a psychological reliance. This happens when a child—or even a parent—starts to believe they can't fall asleep without it. This is precisely why melatonin should be a partner to good sleep habits, not a replacement for them.
Can My Child Take Melatonin Every Night?
While melatonin is generally considered safe for short-term use, the goal isn't for it to become a permanent fixture in your nightly routine. Think of it as a tool to help reset your child's internal clock and establish a healthier sleep-wake cycle.
A great strategy many pediatricians recommend is taking a "melatonin holiday." This means taking a break for a few nights or even a couple of weeks to see if your child can fall asleep naturally. It’s the perfect way to check if their body clock is back on track.
What if Melatonin Doesn't Seem to Be Working?
If you're not seeing the results you hoped for, don't give up just yet. More often than not, the issue is either the timing or the dosage. Giving it too late in the evening or using a dose that's too low are two of the most common missteps.
Of course, melatonin isn’t a magic bullet for everyone. If you've worked with your doctor to fine-tune the dose and timing and still aren't seeing any improvement, it might be time to investigate other potential issues. There could be other factors disrupting your child's sleep that melatonin simply can't address.
At the Sachs Center, we know that sleep is just one piece of the ADHD puzzle. If you're looking for a clear, supportive path forward, our expert-led diagnostic evaluations for ADHD and Autism can provide the answers your family deserves. Book your telehealth assessment today.