Have you ever felt a physical sting from a simple critique? A casual comment that sends your mind spiraling into a full-blown panic? If so, you might be familiar with the intense, overwhelming pain of Rejection Sensitive Dysphoria (RSD).
RSD isn't just "being too sensitive." It's a severe, nearly unbearable emotional reaction to rejection, criticism, or even the perception of failure. For those who experience it, the pain is so profound it can feel like a sudden, sharp physical blow. This experience is deeply intertwined with neurodivergent conditions, especially ADHD.
Decoding the Pain of Perceived Rejection
Let's put this into context. Your boss says, "Can we have a chat later?" For most people, this might spark a little curiosity. But for someone with RSD, those six words can instantly trigger a catastrophic spiral. The mind races with worst-case scenarios, convinced that termination is imminent, all accompanied by an internal wave of panic and shame.
This isn't your everyday social anxiety. It’s a lightning-fast emotional shift that can take you from feeling confident and happy to utterly devastated in seconds. To really get a handle on what Rejection Sensitive Dysphoria is, let’s break down the name.
- Rejection Sensitive: This points to a brain that's highly attuned to social cues. It’s like having a superpower for spotting potential disapproval, but the downside is that it often misreads neutral signals as negative ones.
- Dysphoria: This is a Greek word that means "difficult to bear." It’s the perfect term for the profound, intolerable emotional pain that goes far beyond simple sadness or disappointment.
When you put them together, you get a uniquely painful experience that can wreak havoc on relationships, careers, and self-esteem. It's crucial to understand this is a neurological response—not a personal failing or a lack of willpower.
To give you a quick overview, here are the core components of RSD.
RSD at a Glance: Key Characteristics
| Component | Description |
|---|---|
| Definition | An extreme, painful emotional reaction to perceived or real rejection, criticism, or failure. |
| Primary Triggers | Minor critiques, neutral comments misinterpreted as negative, feeling misunderstood, or falling short of personal or external standards. |
| Typical Reaction | Sudden mood shifts, intense feelings of shame and humiliation, catastrophic thinking, and a feeling of physical pain from emotional distress. |
This table shows just how quickly a seemingly small event can trigger a massive internal reaction.
The Neurological Roots of RSD
At its core, RSD is tied to emotional dysregulation, a hallmark of the ADHD brain. The parts of the brain responsible for processing social feedback and managing emotions just work differently. Think of it as having an emotional smoke alarm with the sensitivity cranked all the way up—it sounds a five-alarm fire for a piece of burnt toast.
Because of this wiring, the pain of rejection isn't just an abstract thought; it’s a visceral, almost physical sensation. This intensity is what makes it such a significant challenge for so many neurodivergent individuals.
Rejection Sensitive Dysphoria is an intense emotional response to perceived or real rejection, most commonly linked to ADHD, where around 99% of individuals experience it. For about one-third of them, RSD is the most debilitating part of their condition. Explore more about the connection between RSD and ADHD.
This intense reaction often leads to coping mechanisms that, unfortunately, create a self-fulfilling prophecy. Someone terrified of rejection might become a people-pleaser, overwork themselves to appear flawless, or simply withdraw from social situations altogether.
While these behaviors are meant to protect against pain, they often lead to burnout, strained relationships, and missed opportunities. Understanding RSD is the first, most critical step toward breaking this cycle and finding healthier ways to manage its profound impact on your life.
Recognizing the Symptoms of RSD in Daily Life
Knowing the definition of Rejection Sensitive Dysphoria is one thing. Spotting it in the middle of a chaotic Tuesday is something else entirely. RSD doesn’t send a warning shot; it ambushes you, turning a perfectly normal moment into an emotional minefield. The experience is almost always a powerful internal storm before it ever breaks the surface.
Imagine sending a text to a friend and watching the hours tick by without a reply. For most people, it's a minor annoyance. But if you have RSD, that silence can feel like a verdict—a clear sign of abandonment that triggers a painful spiral of self-doubt and worst-case scenarios about the end of your friendship.
These aren't just fleeting feelings. They are powerful emotional and behavioral patterns that dictate how a person moves through the world. Learning to identify them is the first real step toward getting a handle on their impact.
Overwhelming Emotional Responses
The emotional side of RSD is often its most defining feature. The reactions are known for their lightning speed and crushing intensity, feeling less like a shift in mood and more like a sudden, overwhelming force of nature.
A core characteristic is the instantaneous, dramatic mood shift that follows a perceived rejection or criticism. A person can go from feeling confident and happy to feeling utterly worthless in the blink of an eye. This isn't a gradual slide into sadness; it’s a freefall.
This plummet is almost always accompanied by a tidal wave of shame. A minor mistake at work, like a typo in an email, isn't just an error—it feels like a public broadcast of your incompetence. The internal feeling of humiliation can be so intense it feels physically painful.
Common emotional symptoms include:
- Intense feelings of failure for not meeting your own or others' expectations.
- Misinterpreting neutral feedback or even a neutral facial expression as harsh, personal criticism.
- Sudden flashes of rage or anger, often directed inward at yourself but sometimes outward.
- Constant rumination over small social interactions, endlessly scanning them for signs of disapproval.
These emotional storms are often invisible to the outside world, leaving the person feeling profoundly alone in their pain.
For someone with Rejection Sensitive Dysphoria, a simple phrase like "Can we talk later?" from a manager can feel like an impending job loss. The brain doesn't just anticipate the worst-case scenario; it experiences the emotional fallout of that scenario as if it's already happened.
Defensive and Avoidant Behaviors
The intense emotional pain of RSD naturally leads people to develop behaviors designed to prevent rejection at all costs. While these are attempts to protect oneself, they often create more problems than they solve.
One of the most common responses is chronic people-pleasing. This isn't just being nice; it’s an exhausting, continuous effort to be whatever you think other people want you to be. The subconscious goal is to become so agreeable, so helpful, that no one could possibly find a reason to reject you.
On the flip side, another common reaction is total avoidance. A person with RSD might turn down a promotion, avoid dating, or refuse to share their creative work. The fear of potential failure or criticism is so paralyzing that they simply opt out of opportunities for growth and connection, figuring it's safer not to even try. Understanding the triggers for these behaviors is crucial, as they can be surprisingly subtle. You can learn more in our guide on the 10 common triggers for RSD.
The Outward Expression of Inner Turmoil
Sometimes, the internal pain becomes too much to hold in and boils over. These reactions can seem completely out of proportion to the situation, leaving friends, family, and colleagues baffled.
Common reactions include intense shame, crying, outbursts of anger, or completely withdrawing from social contact after even the slightest criticism. Triggers as small as gentle teasing or a delayed text can send someone into a deep, painful rumination. In fact, research shows that about one-third of adults with ADHD consider RSD to be their most impairing symptom, which really highlights its powerful impact.
Ultimately, these emotional and behavioral symptoms lock a person in a vicious cycle. The fear of rejection leads to behaviors that can inadvertently push people away or limit potential, which in turn reinforces the deep-seated belief that you are fundamentally unworthy. Recognizing these patterns is the most empowering step you can take toward breaking the cycle and finding the right support.
The Brain Connection: Why RSD Hits So Hard for ADHD and AuDHD
If you’ve ever felt the overwhelming pain of Rejection Sensitive Dysphoria, you know it’s not just “being too sensitive.” This isn’t a character flaw or a sign of weakness. It’s a direct result of how your brain is wired. To really get what RSD is, we need to look at its neurological roots, which run deep in the neurodivergent brain—especially for those with ADHD and the combined experience of Autism and ADHD (AuDHD).
Imagine your brain's emotional regulation system is like a high-tech home security system. In a neurotypical brain, this system is pretty well-calibrated. It knows the difference between a tree branch tapping on the window and an actual intruder, sounding an alarm that matches the threat.
But for someone with ADHD, it's like the sensitivity dial on that system is broken and stuck on max. The parts of the brain that process emotions and social feedback, like the amygdala and prefrontal cortex, are just communicating differently. A minor event—like a friend not texting back right away—gets processed with the same blaring intensity as a major social disaster. The alarm doesn’t just ring; it triggers a full-scale emotional lockdown.
ADHD and the Emotional Amplifier Effect
This hair-trigger response in the ADHD brain comes down to a few key neurological factors. The brain’s vast communication network, which manages everything from focus to feelings, simply has less of a filter. Emotional reactions happen faster and with way more intensity, often before the rational part of the brain has a chance to step in and say, "Hey, let's think about this."
A major player here is dopamine, the neurotransmitter that’s key for regulating mood, motivation, and feelings of reward. People with ADHD often have differences in their dopamine system, which directly impacts their ability to manage emotional highs and lows.
This neurological setup creates the perfect storm for RSD to flourish. An ambiguous social cue isn’t just confusing; it’s instantly flagged as a threat, setting off a powerful, painful defensive response that feels completely real and justified in the moment.
RSD is a biological reality rooted in brain function. The emotional pain isn't imagined—it's a genuine neurological event. The brain's threat-detection circuits are firing with disproportionate intensity, creating a vicious cycle of fear and avoidance.
The Compounded Challenges of AuDHD
When you add Autism to the mix, creating the AuDHD experience, the vulnerability to RSD gets even more complex. The challenges are layered, creating a uniquely difficult social and emotional landscape to navigate. You can learn more about how these conditions overlap in our guide to adult ADHD and Autism.
People with AuDHD are dealing with both ADHD’s emotional volatility and Autism's inherent challenges with social communication. This combination makes the risk of perceived rejection feel constant and incredibly high-stakes.
Here’s how these layers interact and intensify the experience:
- Social Interpretation Difficulties (Autism): An autistic brain can struggle to accurately read between the lines—missing subtle social cues, body language, or shifts in tone. This creates a constant state of uncertainty about where you stand with people.
- Emotional Dysregulation (ADHD): When a misunderstanding inevitably happens, the ADHD brain's tendency toward intense emotional reactions kicks in. That social uncertainty instantly explodes into a full-blown RSD episode filled with shame, hurt, and anxiety.
- Pattern Recognition Meets Social Anxiety: Autistic brains are brilliant at recognizing patterns. But when the pattern you’ve learned—often from a lifetime of social missteps—is rejection, your brain becomes hyper-vigilant. It starts seeing potential rejection in every interaction, triggering the RSD response preemptively just to protect you.
For someone with AuDHD, a simple conversation can feel like walking through a minefield blindfolded. The constant mental energy spent decoding social rules, paired with the intense fear of the emotional fallout from getting it wrong, is profoundly exhausting. Understanding this brain-based connection is the first step toward reframing RSD—not as a personal failure, but as a legitimate neurological difference that deserves compassion and effective strategies.
How Professionals Diagnose and Differentiate RSD
Getting a clear and accurate diagnosis is the first real step toward managing the intense pain of Rejection Sensitive Dysphoria. But the path to that clarity isn't always a straight line. Here's a key point to understand right away: RSD is not currently a standalone diagnosis in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), the official guidebook clinicians use.
Instead, professionals recognize RSD as a clinical concept—a significant and often debilitating feature of other conditions, most notably ADHD. This means a professional won't diagnose you with RSD itself. They will, however, identify it as a core symptom during a broader mental health evaluation, usually when looking at neurodivergent conditions.
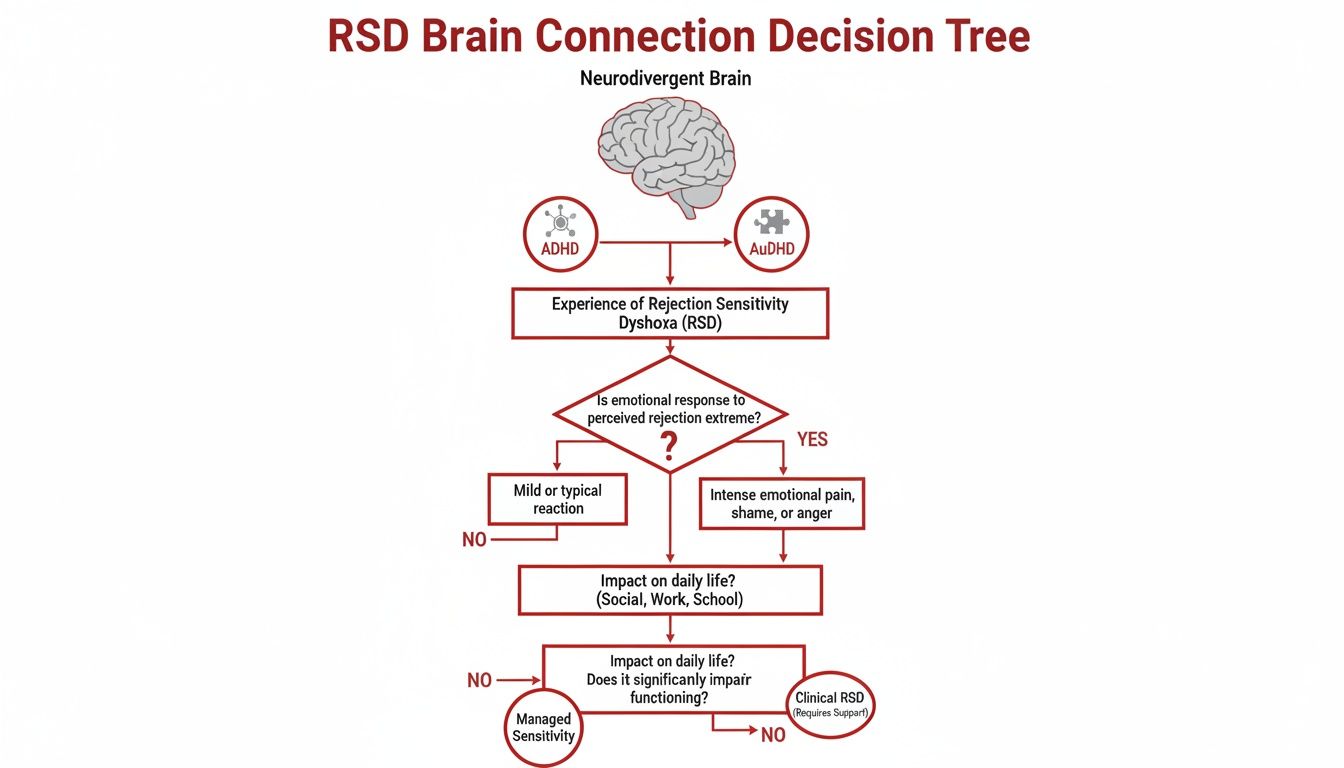
This infographic shows how the neurological wiring in a neurodivergent brain can lead directly to RSD.
As you can see, RSD is often a downstream effect of the emotional dysregulation at the heart of both ADHD and the combined experience of AuDHD.
The Diagnostic Process
Pinpointing RSD isn't about a single test; it's about a careful, comprehensive assessment. A skilled clinician will piece together the puzzle using a few different methods to truly understand your experience.
The process almost always starts with an in-depth clinical interview. During this conversation, your provider will ask detailed questions about your emotional responses to perceived criticism or failure. They’ll want to know how fast these feelings hit, how intense they are, and how long they stick around.
To supplement the conversation, they might use validated self-report questionnaires and symptom checklists. These tools help put numbers to your experiences, comparing them to established clinical patterns linked with ADHD and related conditions. It's the combination of your story and these structured assessments that paints the full picture.
Differentiating RSD from Similar Conditions
One of the most critical parts of this process is what's called a differential diagnosis—basically, telling RSD apart from other conditions with overlapping symptoms. The emotional pain of RSD can look a lot like other disorders from the outside, but the underlying mechanics are completely different. Getting this distinction right is everything when it comes to effective treatment.
A sharp clinician will carefully evaluate the context, triggers, and duration of your emotional pain to find its true source. Without this careful work, you could end up with a treatment plan that doesn't touch the root cause of your distress.
Here are a few common conditions that get mistaken for RSD.
RSD vs. Social Anxiety Disorder
While both involve a fear of social situations, the core fear is worlds apart.
- Social Anxiety: The fear is all about anticipation. It’s a persistent worry about future judgment that builds before and during a social event.
- RSD: The pain is reactive. It’s an immediate, overwhelming emotional gut punch that hits after a perceived rejection has already happened.
RSD vs. Borderline Personality Disorder (BPD)
Both conditions involve a powerful fear of abandonment and intense emotional reactions. However, the emotional shifts in BPD are typically much broader and more prolonged, contributing to a chronic pattern of unstable relationships and self-image. RSD reactions, while incredibly intense, are usually short-lived and tied to a specific triggering event.
The hallmark of an RSD episode is its suddenness and brevity. The extreme emotional pain can feel all-consuming but often dissipates just as quickly as it arrived once the person feels accepted or reassured again.
RSD vs. Depression
A major depressive episode involves a persistent low mood, loss of interest, and feelings of worthlessness that last for at least two weeks. While an RSD episode can certainly trigger feelings of deep sadness and despair, it's a fleeting state. The dysphoric feelings are ignited by a specific event and tend to lift, whereas the mood in depression is a sustained, pervasive state that colors everything.
Understanding these distinctions can empower you to have a much more productive conversation with a healthcare provider. When you can clearly describe what you're going through, you help guide them toward an accurate assessment—and toward support that truly targets the unique challenges of Rejection Sensitive Dysphoria.
Effective Treatments And Therapies For Managing RSD
Living with the intense, gut-punching pain of Rejection Sensitive Dysphoria can feel incredibly isolating, but you are not stuck. There is real hope for managing its impact. The key isn't to stop being sensitive altogether—it's about building the skills to navigate that sensitivity without letting it capsize your life.
The most successful path forward is almost always a personalized, multi-layered plan. This usually involves a combination of medication, targeted therapy, and practical coaching, all developed alongside a professional who truly gets it.
Think of it this way: this combined approach addresses both the brain's wiring and the emotional fallout. It helps calm the overactive neurological alarm system while giving you the psychological tools to handle the signals with intention, not just instinct.
Medication Options To Calm The Nervous System
Because RSD is so deeply tied to the brain’s threat-response system, certain medications can be game-changers. They work by turning down the volume on the emotional storm before it takes over. It's important to know that standard ADHD stimulants don't usually do the trick for RSD, but other non-stimulant medications have shown real promise.
- Alpha-Agonists: Medications like guanfacine and clonidine essentially calm the "fight-or-flight" response in your central nervous system. Imagine them as a dimmer switch for your brain's emotional intensity. They help prevent those rapid, overwhelming reactions that define an RSD episode.
- Monoamine Oxidase Inhibitors (MAOIs): While they're a less common choice due to necessary dietary restrictions, MAOIs can be highly effective for some people when other treatments haven't worked. They help regulate the neurotransmitters involved in mood, which can stabilize the emotional rollercoaster of RSD.
It’s absolutely critical to explore these options with a knowledgeable psychiatrist. Finding the right medication and dosage is a careful, collaborative process that requires professional guidance to be safe and effective.
Therapeutic Approaches For Building Resilience
Therapy is the cornerstone of managing RSD. It creates a safe, structured space where you can start to untangle the catastrophic thought patterns that fuel the pain and begin building new, healthier ways of coping.
The goal of therapy for RSD isn't to stop feeling. It's to stop the feelings from taking complete control. It's about creating that crucial pause between a trigger and your reaction, giving you back the power to choose a different response.
A few therapeutic approaches are particularly well-suited for this work.
Therapy provides the framework for understanding and reshaping your reactions to perceived rejection. Different modalities offer unique tools to build resilience against RSD's powerful emotional pull. The table below breaks down a few of the most effective approaches.
Comparing Therapeutic Approaches for RSD
| Therapy Type | Primary Focus | Key Skills Learned |
|---|---|---|
| Cognitive Behavioral Therapy (CBT) | Identifying and challenging distorted, automatic negative thoughts that fuel RSD episodes. | Thought reframing, reality testing, developing balanced perspectives, and breaking cycles of negative self-talk. |
| Dialectical Behavior Therapy (DBT) | Building concrete skills for emotional regulation and distress tolerance. | Mindfulness, managing intense emotions without reacting impulsively, surviving emotional crises, and improving interpersonal effectiveness. |
Each of these therapies provides a structured way to build the psychological muscle needed to withstand RSD's impact.
- Cognitive Behavioral Therapy (CBT): This approach helps you zoom in on the distorted thoughts that pop up during an RSD flare-up. CBT teaches you to catch automatic negative thoughts—like jumping to "everyone thinks I'm a failure" after a tiny mistake—and challenge them with actual evidence, slowly rewriting your internal script.
- Dialectical Behavior Therapy (DBT): DBT is exceptionally powerful for RSD because it’s all about building a practical toolkit. It teaches you skills in mindfulness, distress tolerance, and emotional regulation, giving you concrete things to do when you're in an emotional crisis so you don't make the situation worse. Learning how to manage intense feelings is a vital step, and you can explore various effective emotional regulation strategies to support this process.
The Role Of Coaching And Practical Skills
Beyond formal therapy, specialized ADHD or neurodiversity coaching can provide invaluable real-time support. A coach helps you take the strategies you learn in therapy and apply them directly to your daily life, whether you're navigating tricky feedback at work or just trying to manage a social gathering.
This practical application is where the change really sticks. A coach can help you develop scripts for difficult conversations, practice advocating for yourself, and build routines that support your emotional stability. For anyone looking for structured guidance, our team has created resources on how to manage Rejection Sensitive Dysphoria, packed with actionable steps you can start using today.
Ultimately, a good treatment plan empowers you to understand your unique brain wiring and work with it, not against it. By combining these approaches, you can transform your relationship with rejection, turning down the pain and turning up your own resilience.
Practical Ways to Find Support and Professional Help
Deciding to get help for Rejection Sensitive Dysphoria can feel like a huge, intimidating first step. But finding the right support is an absolute game-changer. For many, telehealth is an effective and much less stressful way to start, offering a path to expert care without ever leaving home.
If you're neurodivergent, virtual evaluations and therapy can feel a lot more manageable. You’re in your own space, a familiar environment where you have control. This alone can significantly lower the anxiety that bubbles up when you have to talk about sensitive emotional experiences, allowing for a much more open and honest conversation with a provider.
Finding the Right Professional for You
When you start looking for a therapist or clinician, it’s crucial to find someone who gets ADHD and its related challenges—especially RSD. A general therapist might not understand the deep neurological roots of your experience, but a specialist will recognize the unique intensity of RSD and how it’s tangled up with your brain's wiring.
During that first call or consultation, don't be afraid to ask direct questions to see if they’re the right fit:
- How much experience do you have working specifically with Rejection Sensitive Dysphoria?
- What’s your approach to treating RSD for someone with ADHD or AuDHD?
- Do you offer comprehensive diagnostic testing for adult ADHD and Autism?
A good therapeutic relationship is built on feeling seen and truly understood. The right professional will validate what you’re going through, not just brush it off as "being too sensitive." They should create a space where you feel safe enough to explore the deep-seated fears that are driving your RSD.
Finding a professional who understands the nuances of neurodiversity isn’t just a preference; it’s essential. Their expertise ensures that your struggles are met with compassion and proven strategies, not confusion or judgment.
At the Sachs Center, our entire practice is built around specialized telehealth services for neurodivergent individuals. We are experts in diagnosing and treating ADHD and Autism, and that includes understanding the profound impact of what is rejection sensitive dysphoria. Our virtual evaluations are designed to be thorough yet comfortable, giving you a clear path toward the answers and support you’ve been looking for. If you're ready to take that next step, our team is here to help.
Common Questions About Rejection Sensitive Dysphoria
As more people learn about Rejection Sensitive Dysphoria, the questions naturally start to pile up. Trying to make sense of this intense experience can be a lot to handle, but getting clear answers brings validation and a path forward. Let's dig into some of the most common questions to clear up the confusion.
Having solid, reliable information is the first step in reframing the RSD experience—not as a personal flaw, but as a very real neurological challenge.
Can You Have RSD Without Having ADHD?
While RSD and ADHD are very strongly linked, it's not an exclusive relationship. The crushing emotional pain and lightning-fast dysregulation that define RSD can absolutely show up in other conditions, even if the root causes are a bit different.
It can be a major feature for people with:
- Autism Spectrum Disorder (ASD): The challenges of navigating social communication can create a constant state of guesswork, making any perceived rejection feel both frequent and devastating.
- Social Anxiety: While they are distinct, there's a definite overlap. In this case, the deep-seated fear of being judged gets paired with an excruciatingly painful reaction to any perceived criticism.
- Borderline Personality Disorder (BPD): A core feature of BPD is an intense fear of abandonment. The emotional reactions can feel just as powerful as an RSD episode, though they often last longer.
Even so, the sheer prevalence of RSD within the ADHD population is incredibly high, making it a critical piece of the puzzle for any good ADHD diagnosis and treatment plan. The way the ADHD brain is wired creates a unique vulnerability to this kind of emotional whiplash.
How Can I Support a Partner or Friend with RSD?
Supporting someone you care about through an RSD spiral is a delicate dance of compassion, patience, and very clear communication. The most crucial thing to remember is that their emotional pain is 100% real to them, no matter how out of proportion it might look from the outside.
Your validation can be an anchor in their emotional storm. A simple acknowledgment like, "I can see how much that hurt you," is far more effective than trying to rationalize their feelings away.
Try to avoid dismissive phrases like "you're just overreacting" or "don't be so sensitive." Those words are like throwing gasoline on a fire. Instead, focus on validating the feeling while gently holding your own boundaries. Work on communicating with clarity and kindness to minimize the gray areas their brain might misread as rejection. Encouraging them to find professional help and taking the time to learn about RSD yourself are two of the most powerful ways you can show you’re in their corner.
Are There Any Self-Help Strategies That Can Help Immediately?
While getting professional support is the key to long-term management, there are definitely things you can do in the moment to dial down an emotional flood. These aren't magic cures, but they create a vital pause between the trigger and your reaction.
One of the most powerful immediate strategies is reality testing. The second you feel that familiar, gut-wrenching sting of rejection, hit pause and ask yourself a few grounding questions:
- What is the objective, hard evidence that I'm being rejected right now?
- Is there another possible, more neutral way to look at this situation?
- What would I tell a friend if they were in this exact same spot?
Building a mindfulness habit, practicing deep-breathing exercises, and consciously developing a self-compassion practice are also game-changers for countering that harsh inner critic. These tools won't make the sensitivity disappear, but they can give you back a sense of control right when you need it most.
At the Sachs Center, we understand the profound challenges of neurodiversity. Our specialized telehealth services offer expert diagnostic evaluations and treatment for ADHD and Autism, designed to provide clarity and compassionate support. If you are ready to understand your brain better and find effective strategies, explore our services today.