Here's the rewritten section, designed to sound completely human-written and natural, following the provided style guide.
First things first: the main difference between ADD and ADHD is that ADD is an outdated term. While you still hear it used in conversation, it’s no longer a diagnosis medical professionals use. What people used to call ADD is now officially known as ADHD, Predominantly Inattentive Presentation.
From ADD to ADHD: An Evolution in Understanding
The switch from two different terms to one single diagnosis can be a bit confusing, but it comes from a much deeper clinical understanding of the condition. For years, the term Attention Deficit Disorder (ADD) was used for people who struggled mostly with focus, organization, and distractibility, but without the obvious signs of hyperactivity.
But as our diagnostic criteria evolved, clinicians began to see that inattention, hyperactivity, and impulsivity were all symptoms of the same underlying neurodevelopmental condition. The name Attention-Deficit/Hyperactivity Disorder (ADHD) became the official standard because it captures the full range of symptoms.
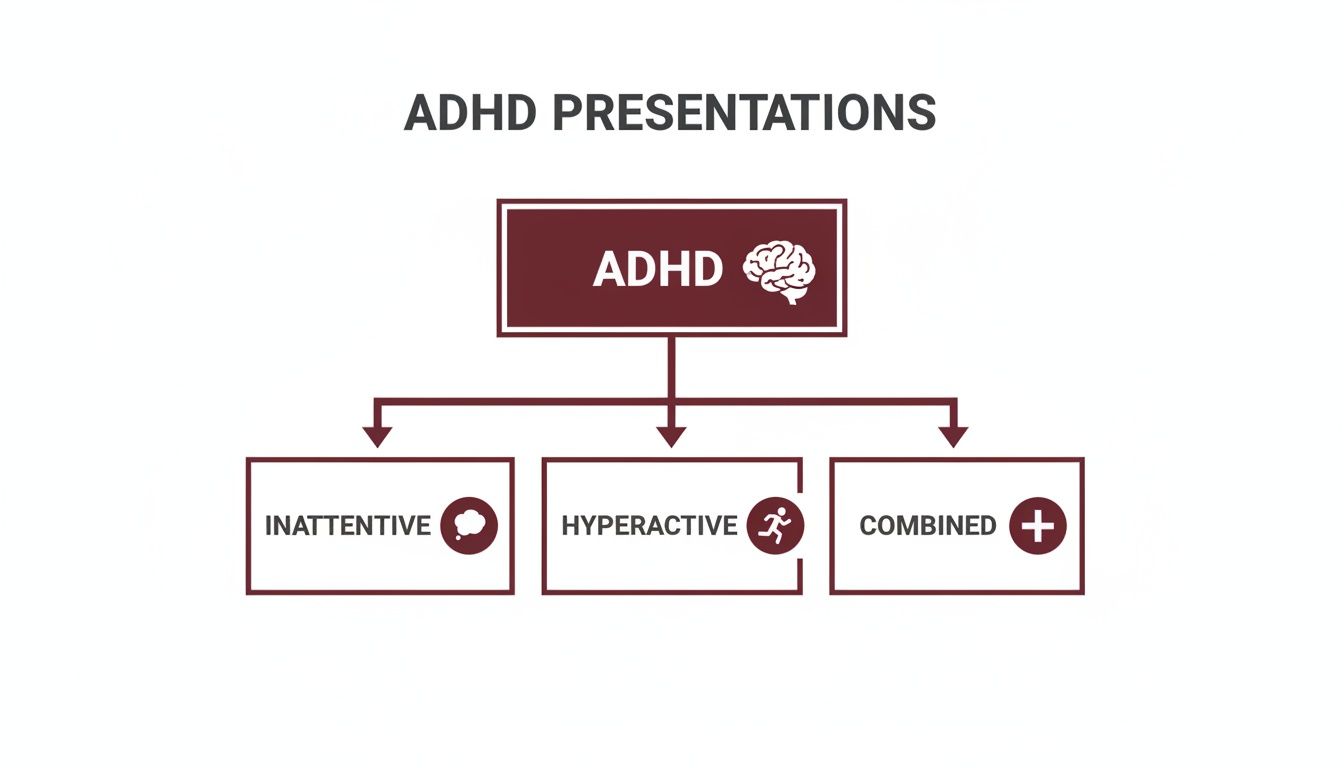
This change was solidified in diagnostic manuals, leading to the current DSM-5, which outlines three distinct presentations of ADHD:
- Predominantly Inattentive Presentation: This is what most people meant when they said ADD. It’s defined by significant challenges with focus, staying organized, and keeping up with mental effort.
- Predominantly Hyperactive-Impulsive Presentation: This presentation is marked by that classic restlessness—an inability to sit still, talking excessively, and acting on impulse without thinking it through.
- Combined Presentation: Someone with this type meets the symptom criteria for both the inattentive and hyperactive-impulsive presentations.
This framework makes it clear that the core issue isn't just about being hyper; it’s about challenges with executive function and self-regulation. The “ADD” label first showed up in the 1980s, but by the time the DSM-IV was published in 1994, it was officially reclassified as a subtype of ADHD to reflect this more complete understanding. You can dig into the historical timeline and prevalence data on this diagnostic evolution over at the National Institute of Mental Health.
Key Takeaway: The conversation is no longer about ADD vs. ADHD. Instead, it's about figuring out which of the three official presentations of ADHD best describes a person's symptoms.
To make this simple, here’s a clear breakdown of the old terminology versus the modern framework we use today.
Historical vs. Modern ADHD Terminology
| Term | Status | Clinical Description |
|---|---|---|
| ADD (Attention Deficit Disorder) | Outdated | Historically described inattentive symptoms without hyperactivity. It's now diagnosed as ADHD, Predominantly Inattentive Presentation. |
| ADHD, Predominantly Inattentive | Current | Characterized by difficulty focusing, disorganization, and forgetfulness. |
| ADHD, Hyperactive-Impulsive | Current | Involves restlessness, impulsivity, and excessive energy. |
| ADHD, Combined Presentation | Current | Meets the criteria for both inattentive and hyperactive-impulsive symptoms. |
As you can see, the shift in language helps us be more precise. It ensures that everyone, whether they're primarily inattentive or hyperactive, is recognized as having a valid form of ADHD.
Exploring the Three Presentations of ADHD
Now that we've cleared up the terminology, let's get into what ADHD actually looks like. It’s not a one-size-fits-all diagnosis. Instead, the DSM-5 outlines three distinct presentations, or subtypes, that capture the different ways symptoms can cluster.
This framework is incredibly helpful because it moves us past the outdated stereotype of a hyperactive little boy. Understanding which presentation fits best is the first real step toward finding strategies that actually work.
This flowchart breaks down how the main diagnosis branches out into its three presentations.
As you can see, ADHD is the core condition, which can manifest as inattentive, hyperactive-impulsive, or a combination of both.
Predominantly Inattentive Presentation
This is the presentation people are usually thinking of when they use the old term "ADD." Someone with this subtype struggles profoundly with focus, organization, and sticking with mentally demanding tasks. They aren't necessarily bouncing off the walls, but inside, their mind can feel like a whirlwind.
Think of the brilliant professional who is constantly losing her keys or the student who seems to "zone out" in class. It's not a lack of interest or intelligence; their brain has just jumped to ten other competing thoughts.
Common symptoms include:
- Making careless mistakes that seem out of character for their ability level.
- Struggling to hold attention during long meetings or conversations.
- Frequently misplacing essential items like a wallet, phone, or important papers.
- Getting easily sidetracked by things others might not even notice.
Because these symptoms are so internal, this presentation is often missed, especially in girls and adult women who become masters at hiding their difficulties.
This quiet, internal struggle is a huge reason why so many adults go undiagnosed. They’ve spent years thinking they’re just "lazy" or "undisciplined," when in reality, they’re dealing with a neurodevelopmental condition.
Predominantly Hyperactive-Impulsive Presentation
This is the presentation that most closely matches the classic ADHD stereotype. It’s defined by a relentless pattern of hyperactivity and impulsivity that gets in the way of school, work, and relationships. It often feels like having an internal motor that simply will not switch off.
This might look like a child who can’t stay seated in the classroom or an adult who constantly interrupts others in conversation, not out of rudeness, but from a genuine struggle with impulse control.
Key signs often include:
- Constant fidgeting, tapping hands, or shaking feet.
- A feeling of being perpetually restless, as if they’re always "on the go."
- Talking excessively or blurting out answers before a question is finished.
- Finding it almost painful to wait their turn in line or in conversations.
Combined Presentation
Just as it sounds, a person with a Combined Presentation meets the diagnostic criteria for both inattentive and hyperactive-impulsive symptoms. This is one of the most frequently diagnosed forms of ADHD.
Living with this presentation means fighting a battle on two fronts. You might struggle to organize your thoughts for a big project at work (inattention) while simultaneously finding it impossible to sit through the kickoff meeting without fidgeting (hyperactivity). This blend of challenges can make navigating structured environments like an office or classroom particularly difficult.
How ADHD Manifests Across Different Demographics
Getting a handle on the difference between the old term ADD and the current diagnosis of ADHD is a great start, but it's really just the beginning. The way ADHD symptoms actually show up in real life is anything but universal—it can look dramatically different depending on someone's age, gender, and even the societal pressures they face. Spotting these variations is absolutely essential for getting an accurate diagnosis and finding support that works.
When most people picture ADHD, they think of a young boy bouncing off the walls in a classroom. That picture isn't wrong, but it's a very narrow slice of the whole pie. Relying on that stereotype is why countless people in other demographics slip through the cracks, never getting the help they need.
The Gender Gap In ADHD Diagnosis
The difference in how ADHD presents between boys and girls is one of the biggest reasons for underdiagnosis. While boys are more likely to show those classic externalizing symptoms—like physical hyperactivity and impulsivity—girls often turn their struggles inward.
This internal experience can look like:
- Intense daydreaming or being called "spacey" (a hallmark of inattention)
- Perfectionism as a way to overcompensate for struggles with organization and planning
- People-pleasing behaviors to avoid being criticized for making a mistake
- Anxiety and depression, which are often the byproduct of a constant, hidden internal battle
Because these symptoms don't disrupt a classroom, they're often dismissed as personality quirks or misdiagnosed as mood disorders. This leads to a massive diagnostic gap. National comorbidity data shows that the lifetime prevalence of ADHD is roughly three times higher in males (13.0%) than females (4.2%). That gap isn't because fewer women have ADHD; it's largely because the inattentive presentations common in girls go unrecognized. You can read more about these epidemiological patterns on Taylor & Francis Online.
For so many women, an ADHD diagnosis doesn't happen until they're well into adulthood, often right after one of their own kids gets diagnosed. They've spent decades thinking they were just lazy or flawed, only to finally discover a neurological reason for their lifelong challenges.
These masked presentations are incredibly complex. You can dive deeper into the unique ways ADHD shows up by reading our guide on the symptoms of ADHD in women.
How Symptoms Evolve From Childhood To Adulthood
ADHD symptoms don't just stay the same; they shift and change as we get older. The very obvious hyperactivity of a young child often morphs into something much more subtle in adulthood, as people learn to cope and face entirely new life demands.
That kid who could never, ever stay in his seat? He might grow into an adult who feels a constant, humming sense of internal restlessness. This could lead him to a high-pressure, fast-paced career, or it might just look like fidgeting nonstop during meetings and being completely unable to relax.
This table gives a clearer picture of how those core symptoms can transform over a lifetime.
Symptom Presentation Across Life Stages
| Symptom Cluster | Common Manifestation in Childhood | Common Manifestation in Adulthood |
|---|---|---|
| Hyperactivity | Running, climbing, unable to sit still | Internal restlessness, fidgeting, choosing a highly active job, feeling easily bored |
| Impulsivity | Blurting out answers, interrupting, difficulty waiting for a turn | Making rash decisions (financial, career), speaking without thinking, risky behaviors |
| Inattention | Losing homework, daydreaming in class, careless mistakes | Chronic disorganization, missing deadlines, trouble with long-term projects, "zoning out" during conversations |
It’s so important to recognize these more nuanced presentations. An adult who's struggling with chronic underemployment, messy finances, and chaotic relationships might not see themselves in the "ADHD kid" stereotype at all, but the underlying neurobiology is exactly the same.
Navigating the ADHD Diagnostic Process
Figuring out that you might have ADHD is the first step. Getting an accurate diagnosis is the crucial next one. This isn’t about taking a quick online quiz; a real evaluation is a deep dive, a structured process designed to give you true clarity about how your unique brain is wired.
A comprehensive ADHD assessment isn't just a single test or a quick chat. It's a multi-faceted approach where a skilled clinician puts together a complete picture of your cognitive and behavioral patterns. Nothing gets missed.
Key Components of an Evaluation
The journey almost always starts with a detailed clinical interview. This is where your clinician gets the full story—your developmental, medical, and family history. They'll ask about your experiences in childhood, school, work, and relationships to see if there are lifelong patterns that point toward ADHD.
After that, you'll likely work through a series of standardized rating scales. These aren't just generic questionnaires. They are evidence-based tools that help quantify your symptoms by comparing your experiences to those of the neurotypical population, adding objective data to your personal story.
An accurate diagnosis isn't just about spotting ADHD symptoms. It's also about ruling out other conditions. Many symptoms of anxiety, depression, and even certain learning disabilities can look a lot like ADHD, which makes a differential diagnosis absolutely essential.
Why a Thorough Process Matters
An experienced diagnostician knows that your symptoms don't exist in a vacuum. That’s why they often gather collateral information—insights from a spouse, parent, or close friend. This gives them an outside perspective on how you show up in daily life, which is especially helpful for adults who might not remember their childhood behaviors clearly.
The evaluation also has to measure your symptoms against established clinical guidelines. Clinicians use specific criteria to figure out if your challenges with inattention or hyperactivity-impulsivity are significant enough to warrant a diagnosis. To get a better sense of what professionals are looking for, you can explore the official ADHD diagnostic criteria used in clinical practice.
Ultimately, the process is about synthesizing all this information—the interviews, the rating scales, and the reports from others—to arrive at a clear conclusion. This isn't just about getting a label. It’s about finally understanding the "why" behind your struggles, turning uncertainty into empowering knowledge that lays the foundation for a truly personalized and effective management plan.
Building an Effective ADHD Management Plan
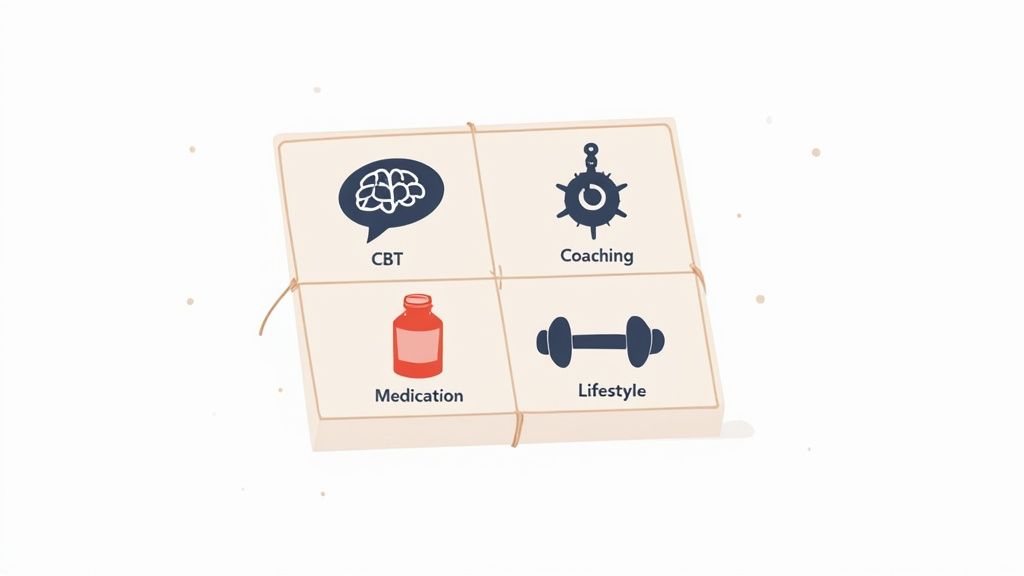
Successfully managing ADHD isn’t about finding a single magic bullet. It's about building a personalized, multi-faceted plan that truly fits your unique needs and challenges. An effective strategy weaves together behavioral therapies, practical skill-building, and smart lifestyle adjustments.
Medication can be an important piece of the puzzle, but it works best as a supportive tool, not the entire plan. This comprehensive approach empowers you to not only manage the tough stuff but also lean into your inherent strengths.
Core Therapeutic Strategies
Cognitive Behavioral Therapy (CBT) is often a cornerstone of ADHD treatment for a reason. It directly helps you identify and reframe the negative thought patterns that can build up after years of ADHD-related struggles—feelings of failure, low self-esteem, or constant self-criticism. CBT gives you practical tools for tackling procrastination, regulating intense emotions, and getting a handle on time management.
Alongside therapy, executive function coaching provides targeted, real-world support for the skills ADHD directly impacts. A coach helps you build personalized systems for organization, planning, and just getting started on tasks. These skills are absolutely crucial for navigating the demands of school, work, and daily life. You can learn more about how this type of coaching builds essential life skills in our guide to ADHD and executive function.
"A holistic ADHD management plan acknowledges that ADHD is not just a deficit of attention, but a complex challenge of regulation. The goal is to build a supportive scaffold of skills, strategies, and therapies that allow the individual's natural abilities to shine through."
The Role of Medication and Lifestyle
For many, medication is a highly effective part of an ADHD management plan. Both stimulant and non-stimulant medications work by balancing brain chemicals to sharpen focus and dial down impulsivity. They create the space needed for other strategies to take root, which is why they’re most powerful when paired with therapy and coaching that teach lasting skills.
Lifestyle adjustments also play a huge role. Things like consistent routines, regular exercise, a balanced diet, and getting enough sleep are all proven to help manage ADHD symptoms. This broader view of treatment is becoming more critical as awareness grows. While diagnoses in children held steady between 2017-2022, some data shows that adult diagnoses have shot up by about 123% over the last decade. This highlights a massive shift in recognizing that ADHD doesn't just disappear after childhood. You can explore more data on these trends in a study published by JAMA Network Open.
When to Seek a Professional ADHD Evaluation
Knowing when to get help is often the hardest part. The line between everyday struggles and something more significant can feel blurry, leaving you wondering if what you’re going through is “bad enough” for an evaluation. But if you consistently feel like your efforts just don't match your results, that's a sign worth looking into.
This feeling often shows up in specific, frustrating patterns. Maybe you’re a smart, capable professional who keeps missing deadlines or making simple mistakes, leading to chronic underperformance no matter how many hours you put in. Or perhaps it’s the constant friction in your relationships because you forget important dates or find your mind wandering during a serious conversation.
It’s Not a Lack of Willpower
These aren't just occasional slip-ups; they’re part of a pattern that can chip away at your self-esteem and leave you feeling completely overwhelmed by daily life. If this rings a bell, a professional evaluation isn’t about getting a label—it's about finally getting an explanation.
Think about whether these common signals sound like you:
- A lifelong sense of being “different” or never quite living up to your potential.
- Chronic disorganization that tangles up your finances, home, or work life.
- Emotional volatility, where small frustrations feel like they trigger a huge reaction.
- Feeling drained from the sheer mental effort it takes just to stay on track.
If you're nodding along to these points, it’s a strong indicator that your struggles might have a neurological basis. An evaluation gives you the clarity to stop blaming yourself and start finding strategies that actually work.
Recognizing these signs is the first step. When the gap between what you know you can do and what you actually do becomes a source of distress, seeking an expert assessment is an act of self-care. At the Sachs Center, our telehealth evaluations are designed to offer that clarity, helping you understand the "why" behind your challenges in a supportive, accessible way.
Your ADHD Questions, Answered
As you explore what ADHD means, a lot of questions are bound to come up. It's completely normal. Here, we'll tackle some of the most common ones to give you a clearer picture of diagnosis, symptoms, and what living with ADHD can really look like.
Can Someone Have Both Inattentive and Hyperactive Symptoms?
Yes, absolutely. In fact, it's one of the most common diagnoses. This is officially known as ADHD, Combined Presentation, and it means a person meets the criteria for both inattention and hyperactivity-impulsivity.
Someone with this presentation might find themselves struggling to organize their thoughts and stay on task, while at the same time feeling a constant, nagging restlessness or acting on impulse.
Is It Possible to Be Diagnosed with ADHD as an Adult?
Yes, and it's happening more and more. Many adults, particularly women or those with quieter, inattentive symptoms, simply flew under the radar as kids. Their struggles were often chalked up to personality traits rather than a neurodevelopmental condition.
A proper adult evaluation is thorough. It involves looking back across your entire life to see if the patterns of ADHD have been there all along, even if no one had the language for it back then.
A lot of adults only start connecting the dots after their own child is diagnosed. That "aha" moment, where they see their own lifelong struggles reflected in their child's experience, is a very common—and powerful—reason to finally seek answers.
Does ADHD Treatment Always Mean Medication?
Not at all. Medication is just one tool in the toolbox, and it's not the right fit for everyone. The most effective ADHD management plans are rarely one-size-fits-all.
Instead, a great approach is often multimodal, bringing together different strategies. This could include behavioral therapy (like CBT), executive function coaching to build practical skills, and simple lifestyle adjustments. The best treatment is always tailored to your specific challenges and what you want to achieve.
And as our understanding grows, so do the resources available. Innovative technologies are even starting to play a role. For instance, new tools like Chatbots for Healthcare are being developed to help people get the information and support they need more easily.
At the Sachs Center, our expertise lies in providing clear, compassionate evaluations to help you find the answers you deserve. If these questions hit home for you or someone you care about, the next step toward clarity is within reach. Learn more about booking a telehealth ADHD evaluation with our team by visiting us at https://sachscenter.com.